Full Citation:
Wolf, EJ. (2013). The Dissociative Subtype of PTSD: Rationale, Evidence, and Future Directions. PTSD Research Quarterly; 24(4).
The Dissociative Subtype of PTSD: Rationale, Evidence, and Future Directions
Erika J. Wolf
National Center for PTSD at VA Boston Healthcare System
Boston University School of Medicine, Department of Psychiatry
The diagnosis of PTSD has undergone numerous changes in the recently released Diagnostic and Statistical Manual-5 (DSM-5; APA, 2013). One is the addition of the dissociative subtype (see Friedman, Resick, Bryant, and Brewin, 2011). This subtype applies to individuals who meet full criteria for PTSD and also exhibit marked symptoms of derealization (i.e., perceiving one’s world or environment as not real) and/or depersonalization (i.e., perceiving one’s self as not whole, connected, or real). This review examines the evidence for the dissociative subtype of PTSD, discusses issues related to its operational definition and assessment, and considers its broader relevance for clinical and research applications.
To begin, it is important to define the term “subtype” and clarify how it is used in DSM-5. In general, the term implies a subordinate variant of a more general kind such that one might expect differences in the core symptoms of a disorder as a function of subtype. However, in this case, the dissociative subtype is not a subset of the core PTSD symptoms, but instead, reflects a form of PTSD marked by additional comorbid symptoms of derealization and/or depersonalization. Most broadly, the term reflects the finding that only a distinct minority of individuals with PTSD experience symptoms of derealization and depersonalization and this is relatively unrelated to the severity of their PTSD symptoms.
Empirical support for the subtype comes from converging lines of research, including psychometric and neurobiological studies. A series of articles have used structural analytic models to examine the distribution of dissociation symptoms within trauma-exposed and PTSD samples. Structural analyses, such as taxometric procedures and latent profile analyses, are ideally suited for testing subtype hypotheses because these analyses take a multivariate approach to examine if there are unobserved, or latent, constructs that distinguish groups of individuals based on their scores on a series of items submitted to the analysis. In the case of latent profile analysis, competing models can be tested and compared against each other using multiple indicators of model fit and substantive interpretability. Waelde, Silvern, and Fairbank (2005) used taxometric procedures to examine the structure of dissociation (as defined by amnesia, depersonalization, and absorption) among trauma-exposed Vietnam Veterans and found that 32% of those with PTSD could be classified as belonging to a dissociative taxon or group. Wolf, Miller et al. (2012) subsequently used latent profile analysis of items indexing PTSD and dissociative symptom severity (as defined by depersonalization, derealization, and reduction in awareness), and demonstrated that about 12% of Veterans with PTSD scored uniquely high on symptoms of derealization and depersonalization. These individuals formed a dissociative class who were distinct from those with high PTSD severity and no dissociation and from those with low PTSD severity and no dissociation. The dissociative group was also associated with higher severity of clinician-rated flashbacks and self-reported a higher level of exposure to childhood and adult sexual assault compared to the other groups. This basic pattern of latent profile results was subsequently replicated in all male and all female veteran and military PTSD samples (Wolf, Lunney et al., 2012). Approximately 15% of the male sample and 30% of the female sample were assigned to the dissociative class, which was again defined by symptoms of depersonalization and derealization. The female dissociative class was associated with higher prevalence of borderline and avoidant personality disorder diagnoses. Steuwe, Lanius, and Frewen (2012) extended this work into a civilian sample of individuals with PTSD and a high prevalence of sexual trauma and found remarkably similar results that latent profile analyses revealed that approximately 25% of the sample could be classified as belonging to a dissociative subgroup, as defined by high scores on derealization and depersonalization. Finally, Stein et al. (2013) contributed an important study of the dissociative subtype in a sample of over 25,000 individuals from 16 different countries. The large sample size and cross-cultural representation permitted evaluation of the correlates and generalizability of the subtype. The authors examined the distribution of symptoms of derealization and depersonalization in the sample (but did not use structural models for this purpose) and found that approximately 14% of the sample could be assigned to a dissociative group and that this group also showed elevations on two core PTSD symptoms: flashbacks and psychogenic amnesia. The dissociative class was associated with male sex, childhood-onset PTSD, greater levels of trauma exposure, and higher levels of functional impairment and suicidality as well as comorbid anxiety disorders. Moreover, the study demonstrated that the basic pattern of results replicated across countries that differed in income, providing strong support for the cross-cultural relevance and generalizability of the subtype.
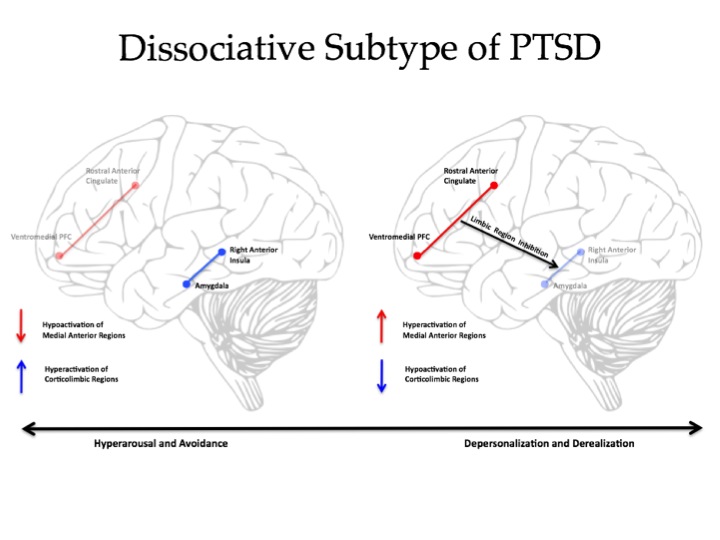
Lanius et al. (2010), followed by Lanius and colleagues (2012), compiled the neurobiological evidence for a dissociative subtype of PTSD. Their review of functional magnetic resonance imaging (fMRI) research suggested that while the majority of individuals with PTSD responded to hearing their personal trauma-scripts with high levels of psychological distress, physiological arousal, emotionality, and reexperiencing, and hyperarousal symptoms, a separate group of individuals responded to hearing their own trauma scripts with a notable absence of such symptoms and instead, showed symptoms of dissociation. The former group was characterized by heightened activity in limbic brain regions (e.g., the amygdala) and reduced activity in areas of the brain associated with emotional control and regulation (largely in pre-frontal regions). In contrast, across studies, Lanius et al. (2010, 2012) noted that the latter group showed evidence of emotional over-modulation, as suggested by heightened activation in pre-frontal brain regions and relatively less activity in the emotional/limbic areas of the brain in response to trauma cues. This provides initial evidence of potential differences in neurobiological functioning in individuals with versus without the subtype, though more research in this area is needed to evaluate the replicability of these patterns of brain activation and their specificity to the dissociative subtype.
Dissociation is a broad term and it is important to highlight that the dissociative subtype of PTSD is formulated based on symptoms of derealization and depersonalization specifically. The focus on these symptoms is consistent with evidence that these types of dissociation reflect more pathological forms of dissociative phenomena that are distinct from other types of dissociation, such as the tendency to “zone out” or have reduced awareness of one’s surroundings. For example, Waller, Putnam, and Carlson (1996) performed taxometric analyses on the Dissociative Experiences Scale (DES; Bernstein and Putnam, 1986), the most widely used measure of dissociative phenomena. Waller et al. showed that some DES items, such as those related to absorption (a trait associated with hypnotizability and cognitive control), reflected dimensional constructs or traits that were relatively nonpathological and normative. In contrast, other items, including those assessing depersonalization and derealization, fit the model for a pathological class or taxon. Others have suggested that symptoms of derealization and depersonalization are facets of a broader form of dissociation termed detachment that is distinct from a form of dissociation termed compartmentalization (which captures phenomena such as dissociative amnesia and symptoms of conversion disorder; see Holmes et al., 2005). The definition of dissociation, its relationship to other constructs, and the key assumptions about the construct are artfully discussed in a critical review by Giesbrech and colleagues (2008) that is required reading for those interested in studying dissociation.
The operational definition of dissociation is important to consider when selecting a measure to assess the dissociative subtype of PTSD. There are many self-report and interview-based measures of dissociation and they vary widely in their approach to the assessment of the construct and in their psychometric properties. The use of dimensional or nonpathological measures of dissociation will be sensitive to normative traits such as absorption, fantasy proneness, and suggestibility that are likely to correlate with PTSD simply as a function of overall severity; their use would be expected to artificially inflate the prevalence of the subtype and fail to identify a unique subgroup. Our group has focused on the use of the associated features items in the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995), the gold standard structured PTSD diagnostic interview, to assess the dissociative subtype. To date, there is no stand-alone instrument that is specific to the dissociative subtype.
The inclusion of the dissociative subtype of PTSD in the DSM-5 has both clinical and research applications. Symptoms of dissociation are important clinical phenomena that may become a target of treatment or may interfere with PTSD treatment. Individuals who are highly dissociative may have difficulty benefitting from trauma-focused therapies if dissociation interferes with the processing of trauma memories and related emotions and cognitions. To date, no study had specifically evaluated if the subtype, as defined in the DSM-5, affects PTSD treatment response or the course of the disorder; most studies evaluating dissociation as a moderator of PTSD treatment response have been under-powered to fully examine this question (as they were not originally designed to address this issue). Two recent studies have provided evidence for subtle differences in PTSD treatment response among individuals with dissociation, though both failed to support an overall dissociation by time interaction on PTSD treatment response. Specifically, Cloitre and colleagues (2012) found that baseline dissociation (broadly defined) did not moderate overall PTSD treatment response, however, dissociation assessed at post-treatment time points did interact with treatment type to yield differential effects on PTSD severity at follow-up. Those with higher levels of post-treatment dissociation fared better with respect to PTSD symptoms if they had been assigned to one of the two treatment arms that involved skills training. Resick et al. (2012) also found no overall dissociation by time effect in predicting response to PTSD treatment but observed that individuals with high levels of dissociation, including symptoms of depersonalization specifically, evidenced a faster decline in PTSD symptoms if they had been assigned to the Cognitive Processing Therapy (CPT) arm of the treatment trial as opposed to the straight cognitive therapy arm (without the written trauma accounts; CPT-C). In other words, although the overall degree of change in PTSD symptoms did not differ as a function of dissociation, the pace, or rate of change in PTSD symptoms, was dependent on dissociative symptoms in combination with treatment type. More work is needed to determine the influence of the dissociative subtype on PTSD treatment response and the best practices for delivering effective PTSD treatment for individuals with salient dissociative symptoms.
The dissociative subtype holds many potential benefits for research purposes. PTSD is a heterogeneous disorder such that any two individuals with the diagnosis may present with different (even nonoverlapping) combinations of PTSD symptoms and patterns of comorbidity. It is important to measure and account for these differences. Otherwise variability in the presentation of PTSD may make it difficult, if not impossible, to identify correlates of the disorder. The dissociative subtype of PTSD may be associated with a distinct etiology, biology, course, and treatment response. For example, individuals with the dissociative subtype may have different genetic vulnerabilities than individuals with PTSD who do not dissociate and failure to account for this phenotypic difference may contribute to statistical “noise” and problems in replicating results across samples. Providing a clear definition of the subtype should allow for research examining the specific genetic, neurobiological, cognitive, and psychosocial mechanisms of dissociation in PTSD.
The association between dissociation and trauma and PTSD has long been a topic of curiosity, speculation, and controversy, and those interested in a historical view may want to read the writings of Pierre Janet dating back to 1889 (and republished in 1973). Controversy about the nature of dissociation in PTSD persists and additional refinement of the definition of the subtype as well as research on its biological and psychosocial correlates and function is still needed. The addition of the subtype in DSM-5 formalizes the PTSD-dissociation relationship and provides a reliable definition of the subtype. This should help to advance the science and understanding of PTSD.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. (Fifth ed.) Arlington, VA: American Psychiatric Association.
- Blake, D.D., Weathers, F.W., Nagy, L.M., Kaloupek, D.G., Gusman, F.D., Charney, D.S., and Keane, T.M. (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75-90.
No comments:
Post a Comment