The Association for Psychological Science has posted this interesting article (which sounds as though it could have been written by the American Psychiatric Association) on Current Status and Future Prospects of Clinical Psychology: Toward a Scientifically Principled Approach to Mental and Behavioral Health Care.
This is yet another call for an evidence-based model of diagnosis and therapy (generally translated as the "medical model" and cognitive-behavioral therapy, CBT) - see here and here for my take on this issue.
Before getting to the main article, here is an editorial comment appearing on the main-page of the ASP Site.
Again, see the articles I linked to above to get a sense of why these issues are not as simple as this brief comment might suggest. A big part of the issue with this is that insurance companies only pay for a limited number of sessions, so the "empirically-proven treatments" are those that can be accomplished in this limited time-frame and which will produce a reduction in symptoms.Current Status and Future Prospects of Clinical Psychology
Toward a Scientifically Principled Approach to Mental and Behavioral Health CareTimothy B. Baker, Richard M. McFall, and Varda Shoham
Over the past 20 years, the prevalence of mental health disorders has nearly doubled in the United States. Yet despite the number of empirically supported treatments now available for a variety of disorders, most clinical psychologists and therapists elect not to use them or rely on out-of-date procedures. Some of these clinicians, coming out of training programs that did not use or teach these scientifically supported methods, may not even be aware of how effective such treatments can be.
For their part, many patients with mental health problems do not even seek help from psychologists; mental health treatment has become so expensive that many patients bypass this route completely, instead seeking out treatment from medical doctors who are covered by their insurance. There, the patients will, in all likelihood, just receive a prescription for a pharmaceutical, when they may actually get better results from a treatment program that incorporates behavioral therapy, managed by a clinical psychologist.
This major new PSPI report, “Current Status and Future Prospects of Clinical Psychology: Toward a Scientifically Principled Approach to Mental and Behavioral Health Care,” aims to address this state of affairs and achieve for the field of clinical psychology what the Flexner Report accomplished for medicine nearly a century ago. Distinguished clinical researchers Timothy Baker (University of Wisconsin-Madison), Richard McFall (Indiana University), and Varda Shoham (University of Arizona) document the urgent need for reforming clinical psychology training in order to ensure that mental health treatment rests on firm empirical foundations. Among their recommendations is a new accreditation system that will help regulate and standardize clinical psychology training programs. Training programs vetted by the new Psychological Clinical Science Accreditation System (PCSAS) will emphasize high-quality, rigorous, and science-based training to ensure that mental health care consumers will consistently receive empirically-proven treatments. Patients and their families will be the direct beneficiaries of this new accreditation system, but the benefits will also extend to insurers and to the public’s welfare more generally.
However, these approaches, empirically-based or not, are not necessarily the BEST treatments. As often as not, long-term depth therapies produce lasting change:
Keep this in mind as I quote from the longer article. Here is a lengthy section from the beginning of the article.Psychodynamic psychotherapy is effective for a wide range of mental health symptoms, including depression, anxiety, panic and stress-related physical ailments, and the benefits of the therapy grow after treatment has ended, according to new research published by the American Psychological Association.
Psychodynamic therapy focuses on the psychological roots of emotional suffering. Its hallmarks are self-reflection and self-examination, and the use of the relationship between therapist and patient as a window into problematic relationship patterns in the patient's life. Its goal is not only to alleviate the most obvious symptoms but to help people lead healthier lives.
"The American public has been told that only newer, symptom-focused treatments like cognitive behavior therapy or medication have scientific support," said study author Jonathan Shedler, PhD, of the University of Colorado Denver School of Medicine. "The actual scientific evidence shows that psychodynamic therapy is highly effective. The benefits are at least as large as those of other psychotherapies, and they last."
OK, that's all I am going to post (formatting text from a PDF is a pain in the arse). Go read the whole position paper.Current Status and Future Prospects of Clinical PsychologyTimothy B. Baker,1 Richard M. McFall,2 and Varda Shoham3
Toward a Scientifically Principled Approach to Mental and Behavioral Health Care
1University of Wisconsin–Madison, 2Indiana University, and 3University of Arizona
SUMMARY—The escalating costs of health care and other recent trends have made health care decisions of great societal import, with decision-making responsibility often being transferred from practitioners to health economists, health plans, and insurers. Health care decision making increasingly is guided by evidence that a treatment is efficacious, effective–disseminable, cost-effective, and scientifically plausible. Under these conditions of heightened cost concerns and institutional–economic decision making, psychologists are losing the opportunity to play a leadership role in mental and behavioral health care: Other types of practitioners are providing an increasing proportion of delivered treatment, and the use of psychiatric medication has increased dramatically relative to the provision of psychological interventions.
Research has shown that numerous psychological interventions are efficacious, effective, and cost-effective. However, these interventions are used infrequently with patients who would benefit from them, in part because clinical psychologists have not made a convincing case for the use of these interventions (e.g., by supplying the data that decision makers need to support implementation of such interventions) and because clinical psychologists do not themselves use these interventions even when given the opportunity to do so.
Clinical psychologists’ failure to achieve a more significant impact on clinical and public health may be traced to their deep ambivalence about the role of science and their lack of adequate science training, which leads them to value personal clinical experience over research evidence, use assessment practices that have dubious psychometric support, and not use the interventions for which there is the strongest evidence of efficacy. Clinical psychology resembles medicine at a point in its history when practitioners were operating in a largely prescientific manner.
Prior to the scientific reform of medicine in the early 1900s, physicians typically shared the attitudes of many of today’s clinical psychologists, such as valuing personal experience over scientific research. Medicine was reformed, in large part, by a principled effort by the American Medical Association to increase the science base of medical school education. Substantial evidence shows that many clinical psychology doctoral training programs, especially PsyD and for-profit programs, do not uphold high standards for graduate admission, have high student–faculty ratios,de-emphasize science in their training, and produce students who fail to apply or generate scientific knowledge.
A promising strategy for improving the quality and clinical and public health impact of clinical psychology is through a new accreditation system that demands high quality science training as a central feature of doctoral training in clinical psychology. Just as strengthening training standards in medicine markedly enhanced the quality of health care, improved training standards in clinical psychology will enhance health and mental health care. Such a system will (a) allow the public and employers to identify scientifically trained psychologists; (b) stigmatize ascientific training programs and practitioners; (c) produce aspirational effects, thereby enhancing training quality generally; and (d) help accredited programs improve their training in the application and generation of science. These effects should enhance the generation, application, and dissemination of experimentally supported interventions, thereby improving clinical and public health. Experimentally based treatments not only are highly effective but also are cost-effective relative to other interventions; therefore, they could help control spiraling health care costs. The new Psychological Clinical Science Accreditation System (PCSAS) is intended to accredit clinical psychology training programs that offer high quality science-centered education and training, producing graduates who are successful in generating and applying scientific knowledge. Psychologists, universities, and other stakeholders should vigorously support this new accreditation system as the surest route to a scientifically principled clinical psychology that can powerfully benefit clinical and public health.
INTRODUCTION
The principal goals of clinical psychology are to generate knowledge based on scientifically valid evidence and to apply this knowledge to the optimal improvement of mental and behavioral health. The primary aims of this monograph are to assess where we stand as a field in achieving these goals and to identify factors that might have limited progress toward their attainment. A secondary aim is to suggest one strategy—the development of a new accreditation system—that might help clinical psychology advance more quickly as an applied science. Undoubtedly, other steps will foster this advance; the discussion of a new accreditation system is offered merely as one example of the bold action that is needed for clinical psychology to meet its obligations to the public. Finally, although we use the term clinical psychologist throughout, our remarks are relevant to all psychologists concerned with clinical service delivery (e.g., assessment or intervention) in the service of clinical and public health.
CLINICAL PSYCHOLOGY IN THE CONTEXT OF PUBLIC HEALTH: ADDRESSING SOCIETY’S NEEDS
The status of clinical psychology cannot be evaluated in isolation; to be understood, it must be viewed in the broader context of contemporary health care. The evidence is clear that we are facing a health care crisis in the United States, and that the nature of health and mental health care has changed dramatically since clinical psychology began in this country. These changes have clear implications for the future of clinical psychology.
* Health and mental health care costs have escalated dramatically over the past 30 years (Centers for Medicare and Medicaid Services, 2006; Mark, Levit, Buck, Coffey, & Vandivort-Warren, 2007; National Center for Health Statistics, 2006; Poisal et al., 2007), and there is little reason to believe that this trend will slow even with greater government intervention and control. This is because these escalating costs reflect somewhat refractory influences: people living longer and requiring greater levels of care, new medical procedures, and a growing number of treatable conditions.
* The rising costs of health and mental health care mean that individuals no longer pay for such care directly: Costs are being diverted to insurers and the government. This means that providers and consumers are losing control over health care decisions; such decisions increasingly are influenced by other stakeholders: for example, health care administrators, purchasers of health plans (e.g., businesses), and insurers.
* Cost pressures and new pharmacotherapies have changed the face of mental health care. The proportion of the population receiving mental health care has almost doubled in the past 20 years (Druss, 2006; Kessler et al., 2005), but increasingly this care is delivered by primary care (medical) practitioners and involves pharmaceuticals (Mark et al., 2007; Olfson, Marcus, Druss, & Pincus, 2002; Zuvekas, 2005).
* While the demand for mental health care is growing, psychologists are being bypassed as practitioners (e.g., Clay, 1998; Committee on Redesigning Health Insurance Performance Measures Payment and Performance Improvement Programs, 2006; Hanrahan & Sullivan-Marx, 2005; Mark et al., 2007). Clinical psychologists are being ‘‘crowded out’’ of service delivery roles by primary care physicians, on one side, and by lower-cost practitioners, such as social workers, on the other side (Scheffler, Ivey, & Garrett, 1998). The training of psychologists has continued apace, however, with some 2,400 new doctoral-level providers being produced each year (Scheffler et al., 1998).
The combination of unmet mental health needs, the escalating costs of mental health treatment, and the use of public monies, puts tremendous pressure on those who make health care decisions to pay careful attention to evidence of costs and effectiveness. Stakeholders in mental health care systems increasingly are using health economic evidence to guide their decision making (Beecham et al., 1997). The professional disciplines and treatments that flourish in the future will be those that are relatively cost-effective, that demonstrate a clear cost–benefit payout on important objective measures over the relatively short term, and that earn endorsement by clinical practice guidelines in support of their standardization and use. Use of such criteria has led to improved cost-effectiveness in diverse fields of medicine, and a recent Institute of Medicine report stressed that similar quality-improvement strategies must be used in future decisions about mental health care (Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders, 2006). Indeed, the mix of expenditures and delivery systems that has evolved over the past 20 years reflects attention to costs and has increased the reach and cost-effectiveness of mental health treatment (Berndt, 2004; Druss et al., 2006; Frank, Salkever, & Sharfstein, 1991; Mark et al., 2007; McKusick et al., 1998).
Health care has changed dramatically and will change even more. Current trends suggest even greater shifts toward managed care versus fee-for-service, generalist medical providers versus psychologists, general medical hospitals and clinics versus mental health programs, and so on. These trends suggest that psychology, and psychologists, will make decreasing contributions to mental and behavioral health, because psychologists have not made good business and clinical cases for the value of their services and interventions and have not made these cases to the right audiences. The current monograph argues for fundamental reform of psychology and psychological training programs to achieve constructive adaptation to the seismic changes in the nature of health care.
The goal of reform would not be to secure employment for psychologists. Rather, it would be to increase the number of people who are helped by effective psychological interventions. Further, the goal would not be to deprive psychologists of their professional autonomy by encouraging passive acquiescence to the decisions of others. Rather, it would be to encourage a more proactive role for psychologists, one that would generate superior and more compelling research evidence for current and yet-to-be-developed psychosocial treatments.
It is true that clinical psychologists almost certainly will lose battles over professional autonomy. Indeed, they already have. Psychologists should take solace, however, in any effort that generates new knowledge about how to help patients more effectively. This sentiment was voiced by Archie Cochrane, a pioneer British clinical epidemiologist and physician who championed empirical medicine. Early in his career, Cochrane was involved in the care of prisoners with tuberculosis and was troubled by the lack of research on that condition and by the absence of evidence on the effectiveness of treatment:What I decided I could not continue doing was making decisions about intervening (for example pneumothorax and thoracoplasty) when I had no idea whether I was doing more harm than good. I remember reading a pamphlet (I think from the BMA) extolling the advantages of the freedom of British doctors to do whatever they thought best for their patients. I found it ridiculous. I would willingly have sacrificed all my medical freedom for some hard evidence telling me when to do a pneumothorax. (Cochrane & Blythe, 1989; cited in Hill, 2000, p. 1190)Cochrane’s emphasis on evidence-based medicine was harshly criticized by his medical colleagues who preferred freedom to do what they wanted over the need to demonstrate effectiveness (Hill, 2000). However, the weight of evidence and perceived responsibility for public health has largely held sway in medicine. The current context of health care in America (and beyond) demands a higher level of accountability than in the past. Health care decisions should reflect cost-effectiveness data, which index the intervention strategies that reduce human suffering most efficiently, rather than by guild interests or by an unskeptical reliance on customary practices. In this way, the emerging focus on accountability should be welcomed by psychologists, as it is consistent with and supportive of clinical psychology’s two principal goals, as stated at the beginning of this monograph: generating scientific knowledge and applying this knowledge to the optimal improvement of mental and behavioral health.
I should point out that their position paper is directed at doctoral programs in clinical psychology. However, the bulk of therapy being done in the trenches is by masters level therapists - such as the people in my program.
Still, the American Psychological Association and the American Psychiatric Association, as well as the Association for Psychological Science, set the tone for research and therapy - and the DSM is written by doctors from the American Psychiatric Association, all of whom favor the medical model.
The biggest problem with all of this is how these people are defining the psyche - for the most part, all three of these governing bodies are defining the psyche (subjective experience of the client) as a by-product of brain function. This is the standard neuroscientific model. It reduces all subjective experience (the qualia of consciousness) to objective physical states and structures.
On the other hand, many of the psychologies that may appear "ascientific" to the authors of this paper recognize that subjective experience is the most important realm that we should be looking at therapeutically (assuming no biological issues, such as nutritional deficiencies, brain damage, developmental issues, and so on). We don't ask the client, "So, how are your amygdala and hippocampus today?" We ask, rather, "How are you feeling today?" or "What's on your mind?"
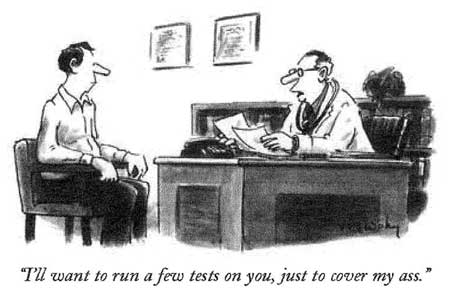
The cognitive behavioral model (the dominant evidence-based therapy) looks at thoughts as objects similar to behaviors, and wants to mold them accordingly. More to the point, this model pits the therapist as expert against the client as patient - a top-dog/under-dog model (to reference Gestalt Therapy, one of those ascientific models). The therapist is charged with telling the client that his/her cognitions are flawed and then with installing more "reality-based" schemas.
Personally, I could not work with this model as either a client or a therapist.
The client-centered approach of Carl Rogers and Abraham Maslow, of the transpersonal work of Jung and Michael Washburn, or the parts models of Hal and Sidra Stone and
Richard Schwartz, all put the healing of the psyche into the hands of the client. In these models, and for me, the client has the tools and awareness needed to find her/his own path to healing, and our job as a therapist is to be their guide to lead them to themselves.
I hold a bottom-up perspective (client-centered) not the top-down perspective (expert-centered) of psychiatry and the variations of the CBT model of therapy.
More to come on the nature of self in subjective experience (from a William James perspective).
No comments:
Post a Comment