As soon as I read the title of this press release, my brain exploded with a booming, "NOOOOOOOOOO!!!!"
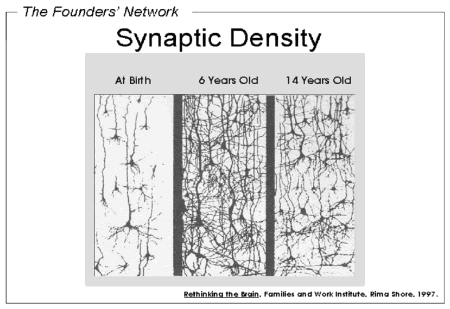
Another study has shown what many of us have long believed to be the source of autism - too many brain synapses that do not get pruned during the first 18 months of life (when the majority of pruning occurs, although there is another period of pruning in adolescence). This explanation makes sense with the old thinking about autism, which suggested that children withdraw, get violent, or tantrum when confronted with interpersonal stimuli and other environmental stimuli because it is overwhelming them. Having too many synapses would explain why it is overwhelming.
But these researchers were not content to know what autism is, they wanted to find the magic pill that would make it all better. What pill can do that, you might ask? Rapamycin, also known as a macrolide produced by the bacteria Streptomyces hygroscopicus. Essentially, it is used to prevent rejection in organ transplants - because it shuts down whole segments of the immune system (T cells and B cells).
What could possibly go wrong? Well, lung toxicity, cancer, and diabetes for starters.
Here is a little explanation of why this is a REALLY BAD idea.
The administration of rapamycin or any similar drug to the brains of infants/toddlers would have indiscriminate effects on the brain - total synapse volume might be reduced, but which synapses will be destroyed, and how would the overall experience of the child be impacted by this?
In normal development, synaptic pruning occurs in response to the child's environment, and one of the most important factors in determining synaptic pruning is the relational environment with the primary caregiver(s).
Here is a little more explanation on this from the book I am currently working on:
Synaptic pruning occurs in the first eighteen months of an infant’s development. Schore (1997) describes the neurobiology of how this restructuring of the brain occurs:[Emphasis added.]
Although the critical period of overproduction of synapses is genetically driven, the pruning and maintenance of synaptic connections [are] environmentally driven. This clearly implies that the developmental overpruning of a corticolimbic system that contains a genetically encoded underproduction of synapses represents a scenario for high risk conditions. (p. 618)“Developmental overpruning” refers to how the release of stress hormones leads to substantial neuronal death as a result of the toxicity of intense stress on the developing brain. Neurons in the important pathways linking the neocortex and limbic system—brain areas that handle emotional regulation—are most affected (Schore, 1996). According to Siegel (2012),
Children who may have a “genetically encoded underproduction of synapses,” or who may have a genetic variant that dysregulates the production of related neurotransmitters such as dopamine, may be at especially high risk if exposed to overwhelming stress. (p. 113)
There are "tens of thousands of new synapses being formed daily during the early years"of a child's development (Sullivan, 2012). At the same time, unused synapses are pruned away. The ones that are lost and the ones that remain are dependent on the experience of the child - the process is context specific, not random. And if it can be addressed without invasive drugs, for example, by learning and experience (both of which are ways the brain creates and releases connections), then why not try this avenue?
From the material above, it is clear that too few synapses also causes development issues, including depression, anxiety, conduct disorder, and lack of impulse control. It's a fine line between too many and too few synapses, and administration of a drug such as rapamycin not only results in random pruning, but may also create too much pruning.
Here is a longer passage from Sullivan on "experience-dependent plasticity":
Experience can determine the selective survival of neurons, the relative complexity of the axonal and dendritic branching, and the number of synapses that exist between cells.While the selection process in synaptic pruning is environmentally (and especially relationally) determined, the impetus of the pruning process is a genetic trigger. In autism, the genetic trigger either is not present or malfunctions. If there is to be ANY kind of intervention, it needs to target the genetic level, and quite possibly the molecular level of gene activity. It certainly should not target the developing brain.
Much of this experience-dependent control of brain development relies upon the experiences either increasing or decreasing the neural activity of a cell. For example, unused neurons (neurons with little neural activity) will die, while used neurons will survive. This is a normal process that occurs in the developing brain—too many cells are born and are then pruned. While new neurons are born in the brain throughout life, the enormity of early life growth is never replicated in later life. The implications of this process for custodial decisions in very early life are enormous—early life deprivation fails to activate neurons, which means that a greater number of neurons will die. Equally important, neurons that would typically die under “normal” conditions could be retained under deprivation or conditions of abuse. In either situation, brain function for the typical social environment in our Western culture might be compromised.
Okay, I now step down from my soapbox. Following the references cited above, here is the press release that got me all bent out of shape in the first place.
References (in order presented):
- Schore, AN. (1997). Early organization of the nonlinear right brain and development of a predisposition to psychiatric disorders. Development and Psychopathology: 9(4): 595–631.
- Schore, AN. (1996). The experience-dependent maturation of a regulatory system in the orbital prefrontal cortex and the origin of developmental psychopathology. Development and Psychopathology; 8(1), 59–87.
- Siegel, DJ. (2012). The Developing Mind, Second Edition: How Relationships and the Brain Interact to Shape Who We Are; 2nd ed. New York: The Guilford Press.
- Sullivan, RM. (2012, Aug). The Neurobiology of Attachment to Nurturing and Abusive Caregivers. Hastings Law J.; 63(6): 1553–1570.
* * * * *
Here is the press release - the whole article is also freely available online.
Children with autism have extra synapses in brain: May be possible to prune synapses with drug after diagnosis
Date: August 21, 2014
Source: Columbia University Medical Center
Summary:
Children and adolescents with autism have a surplus of synapses in the brain, and this excess is due to a slowdown in a normal brain “pruning” process during development, according to a new study. Because synapses are the points where neurons connect and communicate with each other, the excessive synapses may have profound effects on how the brain functions.

In a study of brains from children with autism, researchers found that autistic brains did not undergo normal pruning during childhood and adolescence. The images show representative neurons from autistic (left) and control (right) brains; the spines on the neurons indicate the location of synapses. Credit: Guomei Tang, PhD and Mark S. Sonders, PhD/Columbia University Medical Center
Children and adolescents with autism have a surplus of synapses in the brain, and this excess is due to a slowdown in a normal brain "pruning" process during development, according to a study by neuroscientists at Columbia University Medical Center (CUMC). Because synapses are the points where neurons connect and communicate with each other, the excessive synapses may have profound effects on how the brain functions. The study was published in the August 21 online issue of the journal Neuron.
A drug that restores normal synaptic pruning can improve autistic-like behaviors in mice, the researchers found, even when the drug is given after the behaviors have appeared.
"This is an important finding that could lead to a novel and much-needed therapeutic strategy for autism," said Jeffrey Lieberman, MD, Lawrence C. Kolb Professor and Chair of Psychiatry at CUMC and director of New York State Psychiatric Institute, who was not involved in the study.
Although the drug, rapamycin, has side effects that may preclude its use in people with autism, "the fact that we can see changes in behavior suggests that autism may still be treatable after a child is diagnosed, if we can find a better drug," said the study's senior investigator, David Sulzer, PhD, professor of neurobiology in the Departments of Psychiatry, Neurology, and Pharmacology at CUMC.
During normal brain development, a burst of synapse formation occurs in infancy, particularly in the cortex, a region involved in autistic behaviors; pruning eliminates about half of these cortical synapses by late adolescence. Synapses are known to be affected by many genes linked to autism, and some researchers have hypothesized that people with autism may have more synapses.
To test this hypothesis, co-author Guomei Tang, PhD, assistant professor of neurology at CUMC, examined brains from children with autism who had died from other causes. Thirteen brains came from children ages two to 9, and thirteen brains came from children ages 13 to 20. Twenty-two brains from children without autism were also examined for comparison.
Dr. Tang measured synapse density in a small section of tissue in each brain by counting the number of tiny spines that branch from these cortical neurons; each spine connects with another neuron via a synapse.
By late childhood, she found, spine density had dropped by about half in the control brains, but by only 16 percent in the brains from autism patients.
"It's the first time that anyone has looked for, and seen, a lack of pruning during development of children with autism," Dr. Sulzer said, "although lower numbers of synapses in some brain areas have been detected in brains from older patients and in mice with autistic-like behaviors."
Clues to what caused the pruning defect were also found in the patients' brains; the autistic children's brain cells were filled with old and damaged parts and were very deficient in a degradation pathway known as "autophagy." Cells use autophagy (a term from the Greek for self-eating) to degrade their own components.
Using mouse models of autism, the researchers traced the pruning defect to a protein called mTOR. When mTOR is overactive, they found, brain cells lose much of their "self-eating" ability. And without this ability, the brains of the mice were pruned poorly and contained excess synapses. "While people usually think of learning as requiring formation of new synapses, "Dr. Sulzer says, "the removal of inappropriate synapses may be just as important."
The researchers could restore normal autophagy and synaptic pruning -- and reverse autistic-like behaviors in the mice -- by administering rapamycin, a drug that inhibits mTOR. The drug was effective even when administered to the mice after they developed the behaviors, suggesting that such an approach may be used to treat patients even after the disorder has been diagnosed.
Because large amounts of overactive mTOR were also found in almost all of the brains of the autism patients, the same processes may occur in children with autism.
"What's remarkable about the findings," said Dr. Sulzer, "is that hundreds of genes have been linked to autism, but almost all of our human subjects had overactive mTOR and decreased autophagy, and all appear to have a lack of normal synaptic pruning. This says that many, perhaps the majority, of genes may converge onto this mTOR/autophagy pathway, the same way that many tributaries all lead into the Mississippi River. Overactive mTOR and reduced autophagy, by blocking normal synaptic pruning that may underlie learning appropriate behavior, may be a unifying feature of autism."
Alan Packer, PhD, senior scientist at the Simons Foundation, which funded the research, said the study is an important step forward in understanding what's happening in the brains of people with autism.
"The current view is that autism is heterogeneous, with potentially hundreds of genes that can contribute. That's a very wide spectrum, so the goal now is to understand how those hundreds of genes cluster together into a smaller number of pathways; that will give us better clues to potential treatments," he said.
"The mTOR pathway certainly looks like one of these pathways. It is possible that screening for mTOR and autophagic activity will provide a means to diagnose some features of autism, and normalizing these pathways might help to treat synaptic dysfunction and treat the disease."
The paper is titled, "Loss of mTOR-dependent macroautophagy causes autistic-like synaptic pruning deficits." Other authors are: Kathryn Gudsnuk, Sheng-Han Kuo, Marisa L. Cotrina, Gorazd Rosoklija, Alexander Sosunov, Mark S. Sonders, Ellen Kanter, Candace Castagna, Ai Yamamoto, Ottavio Arancio, Bradley S. Peterson, Frances Champagne, Andrew J. Dwork, and James Goldman from CUMC; and Zhenyu Yue (Icahn School of Medicine at Mount Sinai). Marisa Cotrina is now at the University of Rochester.
Story Source:
The above story is based on materials provided by Columbia University Medical Center. Note: Materials may be edited for content and length.
Journal Reference:
Tang, G, Gudsnuk, K, Kuo, SH, Cotrina, ML, Rosoklija, G, Sosunov, A, Sonders, MS, et al. (2014). Loss of mTOR-Dependent Macroautophagy Causes Autistic-like Synaptic Pruning Deficits. Neuron; Epub ahead of print. DOI: 10.1016/j.neuron.2014.07.040
No comments:
Post a Comment