At the end of a recent BBC article (
Why are we still using electroconvulsive therapy? Jul 24, 2013) on the contemporary use of electroconvulsive therapy (ECT) for treatment-resistant depression, Professor Ian Reid (University of Aberdeen) is quoted as saying, "
No one would be happier than me if we could reproduce the changes that ECT has on the brain in a less invasive and safer way for patients."
Earlier in the article, the reporter offers a brief summary of the current theory of how ECT can be effective in reducing depressive symptoms in those who have not responded to other approaches (mostly pharmaceutical).
The latest theories build on the idea of hyperconnectivity. This new concept in psychiatry suggests parts of the brain can start to transmit signals in a dysfunctional way, overloading the system and leading to conditions from depression to autism.
Prof Reid and his colleagues used MRI scanners to map the brains of nine patients before and after treatment.
In an academic paper in 2012 they claimed ECT can "turn down" overactive connections as they start to build, effectively resetting the brain's wiring. "For the first time we can point to something that ECT does in the brain that makes sense in the context of what we think is wrong in people who are depressed," Prof Reid says.
There is new research (just published this week) that supports the idea that ECT works by disrupting brain activity and neural patterns, essentially acting as a reset for brain function.
Citation:
C. Challis, J. Boulden, A. Veerakumar, J. Espallergues, F. M. Vassoler, R. C. Pierce, S. G. Beck, O. Berton. (2013, Aug). Raphe GABAergic Neurons Mediate the Acquisition of Avoidance after Social Defeat. Journal of Neuroscience; 33 (35): 13978-13988. DOI: 10.1523/JNEUROSCI.2383-13.2013
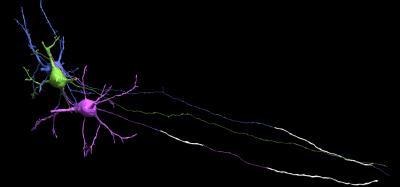
In a recent study, from the lab of Olivier Berton, PhD (assistant professor, department of Psychiatry), in collaboration with Sheryl Beck, PhD (professor, department of Anesthesiology) at Children's Hospital of Philadelphia, the researchers discovered that bullying and similar social stresses (chronic unavoidable stress, or CUS) appear to create symptoms of depression in mice. This stress response activated GABAergic neurons in the dorsal raphe nucleus (DRN), they found, which directly inhibited serotonin levels. With low serotonin levels (although no one has ever determined exactly what those levels might be
[1]), a depressed mouse (and presumably a person) is more likely to be depressed and socially withdrawal.
When the researchers were able to mute the GABA neurons, the mice became more resilient to bullying and didn't avoid once-perceived threats.
"This is the first time that GABA neuron activity -- found deep in the brainstem -- has been shown to play a key role in the cognitive processes associated with social approach or avoidance behavior in mammals," said Dr. Berton. "The results help us to understand why current antidepressants may not work for everyone and how to make them work better -- by targeting GABA neurons that put the brake on serotonin cells."
This where the research into ketamine as a powerful tool in alleviating treatment-resistant depression.
Ketamine is known primarily as a
NMDA receptor noncompetitive antagonist (inhibits action of the NMDA receptor), used most often as an anesthetic, but known to have a wide range of effects in humans, including analgesia, anesthesia, hallucinations, elevated blood pressure, and bronchodilation. Like other drugs of its class, such as
tiletamine and
phencyclidine (PCP), ketamine induces a state referred to as "
dissociative anesthesia" and, known on the street as Vitamin K, is used as a recreational drug.
The development of depressive behaviors, notably
anhedonia (inability to experience pleasure), with CUS
exposure (as in the mice studied above) make CUS one of the most valid
research models for depression. There is already considerable and still building evidence that
glutamate NMDA receptor antagonists can rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure (Li et al.,
Biological Psychiatry, 2011).
From Li, et al:
Chronic stress paradigms have been demonstrated to profoundly alter brain structure and function in rodents, causing atrophy of pyramidal neurons in the PFC and the hippocampus (12,13,15-18,20,32). Studies were conducted to determine if our CUS paradigm results in alterations of synapse-associated proteins, as well as the number and function of spine synapses, and if ketamine can reverse these effects. CUS exposure (21 d) decreased levels of several well-characterized synaptic proteins in synaptoneurosome preparations of PFC (Figure 3).
Administration of single dose of ketamine rapidly reversed the CUS-induced behavioral deficits in various feeding behaviors, as well as restoring CUS-decreased levels of the presynaptic protein synapsin I and the postsynaptic proteins GluR1 subunit and PSD95.
The following is from a paper by Rujescu, et al (2006:
A Pharmacological Model for Psychosis Based on N-methyl-D-aspartate Receptor Hypofunction: Molecular, Cellular, Functional and Behavioral Abnormalities;
Biological Psychiatry; 59:721–729
):
Blocking NDMA receptors leads to an excessive release of glutamate (Glu) in the cerebral cortex (Moghaddam et al 1997). This in turn can have deleterious effects on the blocked neuron as well as on downstream corticolimbic brain regions. The paradox of eliciting increased excitation by blocking an excitatory receptor becomes intelligible in view of the functional interaction of gamma-aminobutyric acid (GABA)ergic (inhibitory) interneurons and glutamatergic (excitatory) neurons in local circuits. Activation of GABAergic interneurons via NMDA receptors exerts an inhibitory tone on the major excitatory neurons (Olney et al 1991). As we have demonstrated, GABAergic interneurons are tenfold more sensitive to NMDA receptor inhibitors than pyramidal neurons (Grunze et al 1996). Application of these agents would therefore result in a disinhibition of pyramidal cell activity with widespread downstream glutamate mediated excitotoxicity through alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) and kainate receptors, which remain largely unaffected by NMDA inhibitors like MK-801 (Ikonomidou et al 1989,1999).
And even if this dysregulation created by blocking (or inhibiting, in the case of ketamine) NMDA receptors was not severe enough to cause structural damage, there are likely to be considerable functional consequences "
because of the crucial role of inhibitory GABAergic output for information processing":
According to in vitro data, GABAergic neurons yield an oscillatory synchronization of anatomically distributed cell groups, which is considered essential for proper integration of temporospatial information in memory operations (Buzsaki and Chrobak 1995; Buzsaki and Draguhn 2004; Ritz and Sejnowski 1997; von der Malsburg 1995).
As discussed in the
Challis, et al article above, CUS causes GABAergic neurons to become much more excitable, which leads to symptoms of depression and anxiety. Increased GABA levels cause a commensurate drop in serotonin levels, which researchers associate with expressions of social defeat, withdrawal, and anhedonia.
Based on the available research, it seems the ketamine "cures" depression so quickly by shutting down the excitability of GABAergic neurons (which become excitable as a result of the organism being exposed to chronic unavoidable stress). Reduced GABA allows for increased serotonin levels, which are associated with "
a positive shift in the perception of socio-affective stimuli, promoting affiliation and dominance."
This is a much more targeted approach than ECT, which likely also shuts down GABAergic neuron excitability, but has a much wider range of effects as well. The brain reset associated with ECT is done much more efficiently with ketamine. Like ECT, ketamine (an anesthetic) also probably generates a "electrocortical quiescence" in the brain that functions as a reset mechanism.
Like ketamine, a newer anesthetic substance, Isoflurane, also seems to demonstrate rapid decreases in depressive symptoms for those who have been unresponsive to other pharmaceutical treatments. From
Wikipedia:
Isoflurane reduces pain sensitivity (analgesia) and relaxes muscles. Isoflurane likely binds to GABA, glutamates and glycine receptors, but has different effects on each receptor. It potentiates glycine receptor activity, which decreases motor function. It inhibits receptor activity in the NMDA glutamate receptor subtype. Isoflurane inhibits conduction in activated potassium channels. Isoflurane also affects intracellular molecules. It activates calcium ATPase by increasing membrane fluidity. It binds to the D subunit of ATP synthase and NADH dehydrogenase.
There is increasing evidence of isoflurane effectiveness in treating major depression.
Citation:
Weeks HR III, Tadler SC, Smith KW, Iacob E, Saccoman M, et al. (2013, Jul 26). Antidepressant and Neurocognitive Effects of Isoflurane Anesthesia versus Electroconvulsive Therapy in Refractory Depression. PLoS ONE 8(7): e69809. doi: 10.1371/journal.pone.0069809
When isoflurane is compared head-to-head with ECT, the outcomes are similar, except that the ECT subjects suffered greater cognitive deficits. Over the course of 3 weeks, patients with "
medication-refractory depression" received an average of 10 treatments of bifrontal ECT (N=20) or an equivalent number of deep-inhalation isoflurane treatments (N=8).
Here is a nice summary of the results from
Medscape Medical News:
Both therapies produced significant (P < .0001) reductions in depression scores on the Hamilton Rating Scale for Depression–24 immediately following the end of treatment, and the benefits persisted at 4 weeks' follow-up. ECT patients had "modestly better" antidepressant effect at follow-up in severity-matched patients, the researchers note.
As expected, ECT caused thinking problems. Immediately after the treatments, ECT patients showed decline in memory, verbal fluency, and processing speed. Most of these ECT-related deficits resolved by 4 weeks. However, autobiographic memory, or recall of personal life events, remained below pretreatment levels for ECT patients 4 weeks after treatment.
In contrast, patients treated with isoflurane showed no performance decrement on any of the traditional cognitive impairment measures at any point. In fact, the isoflurane patients showed significant improvements in some tests, which could be a result of the combined effects of decreased depressive state and practice.
The next step in the research should be a head-to-head, placebo controlled double-blind study comparing isoflurane with ketamine. At the moment, it seems that isoflurane requires more treatments (they used 10 deep-inhalation isoflurane treatments over three weeks in the
PLoS ONE study) than ketamine (a 2012 study used 6 intravenous infusions treatments over two weeks
[2]).
In fact, this second study (Murrough, 2012) postulated a mechanism of action similar to what I have proposed above:
A series of studies found that ketamine and other NMDAR antagonists enhance glutamateric signaling in the cortex of rodents, potentially through inhibition of GABAergic interneurons and subsequent disinhibition of cortical pyramidal neurons (26,27). Enhancement of activity at pyramidal glutamatergic synapses by ketamine would be consistent with the observations of enhanced cortical synaptic plasticity and function described above. Neuroimaging studies in humans likewise suggest that subanesthetic doses of ketamine result in elevated cortical activity, including in regions of PFC and ACC (28–31). A functional MRI (fMRI) study found that ketamine resulted in decreased activity in ventromedial PFC (VMPFC), OFC and SGACC accompanied by increased activity in posterior cingulate and other cortical regions (32).
So while ECT seems to affect much of the brain, which no doubt accounts for the cognitive deficits and the loss of autobiographical memory, ketamine (and presumably isoflurane) dampens activity in the ventromedial prefrontal cortex (vmPFC), the orbital frontal cortex (OFC), and the subgenual anterior cingulate cortex (sgACC), while it also increases activity in the posterior cingulate and other cortical regions.
The vmPFC is associated with emotional processing, decision making and, according to Antonio Damasio (1996)
[3], via
Wikipedia:
the vmPFC has a central role in adapting somatic markers—emotional associations, or associations between mental objects and visceral (bodily) feedback—for use in natural decision making. This account also gives the vmPFC a role in moderating emotions and emotional reactions because whether the vmPFC decides the markers are positive or negative affects the appropriate response in a particular situation.
The sgACC is also associated with emotion regulation (
Drevets, Savitz, and Trimble, 2009), and it shows a size decrease in those with depression:
In a combined positron emission tomography/magnetic resonance imaging study of mood disorders, we demonstrated that the mean gray matter volume of this “subgenual” ACC (sgACC) cortex is abnormally reduced in subjects with major depressive disorder (MDD) and bipolar disorder, irrespective of mood state. Neuropathological assessments of sgACC tissue acquired postmortem from subjects with MDD or bipolar disorder confirmed the decrement in gray matter volume, and revealed that this abnormality was associated with a reduction in glia, with no equivalent loss of neurons. In positron emission tomography studies, the metabolic activity was elevated in this region in the depressed relative to the remitted phases of the same MDD subjects, and effective antidepressant treatment was associated with a reduction in sgACC activity.
The OFC is more of a switching station, processing sensory data from a variety of somatic inputs and sharing extensive connections with other association cortices, primary sensory and association cortices, limbic systems, and other subcortical areas. Corticocortical connections include extensive local projections to and from other prefrontal regions, as well as with motor, limbic, and sensory cortices. Areas projecting to motor areas are densely interconnected with other prefrontal cortical regions, reflecting integration for executive motor control (
Cavada, Company, Tejedor, Cruz-Rizzolo, and Reinoso-Suarez, 2000).
From this it seems that part of the effect of ketamine infusion is a dampening of the parts of the brain associated with emotional regulation, affective processing, and the interplay between somatic states and emotional states. Since isoflurane also seems to work on the glutamate system, it will be interesting to see if it produces the same outcomes and affects the same brain structures and functions.
Bottom line: both ketamine and isoflurane are effective and safer therapeutics for treatment-resistant depression.
NOTES:
1. "There is now substantial evidence that unmedicated depressed patients have abnormalities in brain 5-HT function; however, the relation of these abnormalities to the clinical syndrome is unclear." [Cowen, PJ. (2008, Sep 1). Serotonin and depression: Pathophysiological mechanism or marketing myth?
Trends in Pharmacological Sciences, Volume 29, Issue 9, 433-436. doi:
10.1016/j.tips.2008.05.004]
2. Citation for this study:
Murrough, JW. (2012, Feb). Ketamine as a Novel Antidepressant: From Synapse to Behavior. Clinical Pharmacology & Therapeutics; 91(2): 303–309. Published online 2011 December 28. doi: 10.1038/clpt.2011.244
3. Citation for the Damasio study:
Damasio, AR, Everitt, BJ, Bishop, D. (1996, Oct 29).
The Somatic Marker Hypothesis and the Possible Functions of the Prefrontal Cortex.
Philosophical Transactions: Biological Sciences, Vol. 351, No. 1346, Executive and Cognitive Functions of the Prefrontal Cortex, pp. 1413-1420.