Over at
Scientific American, Gary Stix, Sci Am editor, writer, and blogger at
Talking Back, has posted a 3-part series on research into ketamine as an antidepressant. Right now, any doctor or psychiatrist prescribing ketamine for depression is doing so off-label (i.e., the FDA has not approved that drug as a treatment for that condition). There are an increasing number of clinics who doing just that.
In essence, these doctors are using ketamine (okay, yes, some doctors are probably less than ethical in this realm) as the research suggests has been most useful - slow infusion therapy. But for Big Pharma, there is no money in a chemical that cannot be patented (it's fully available as a generic), so they are tinkering with the chemical structure to make it more effective, more long-lasting, anything, so long as it can be patented as a new chemical.
This is a good series - and it feels like balanced reporting.
By Gary Stix | September 11, 2013
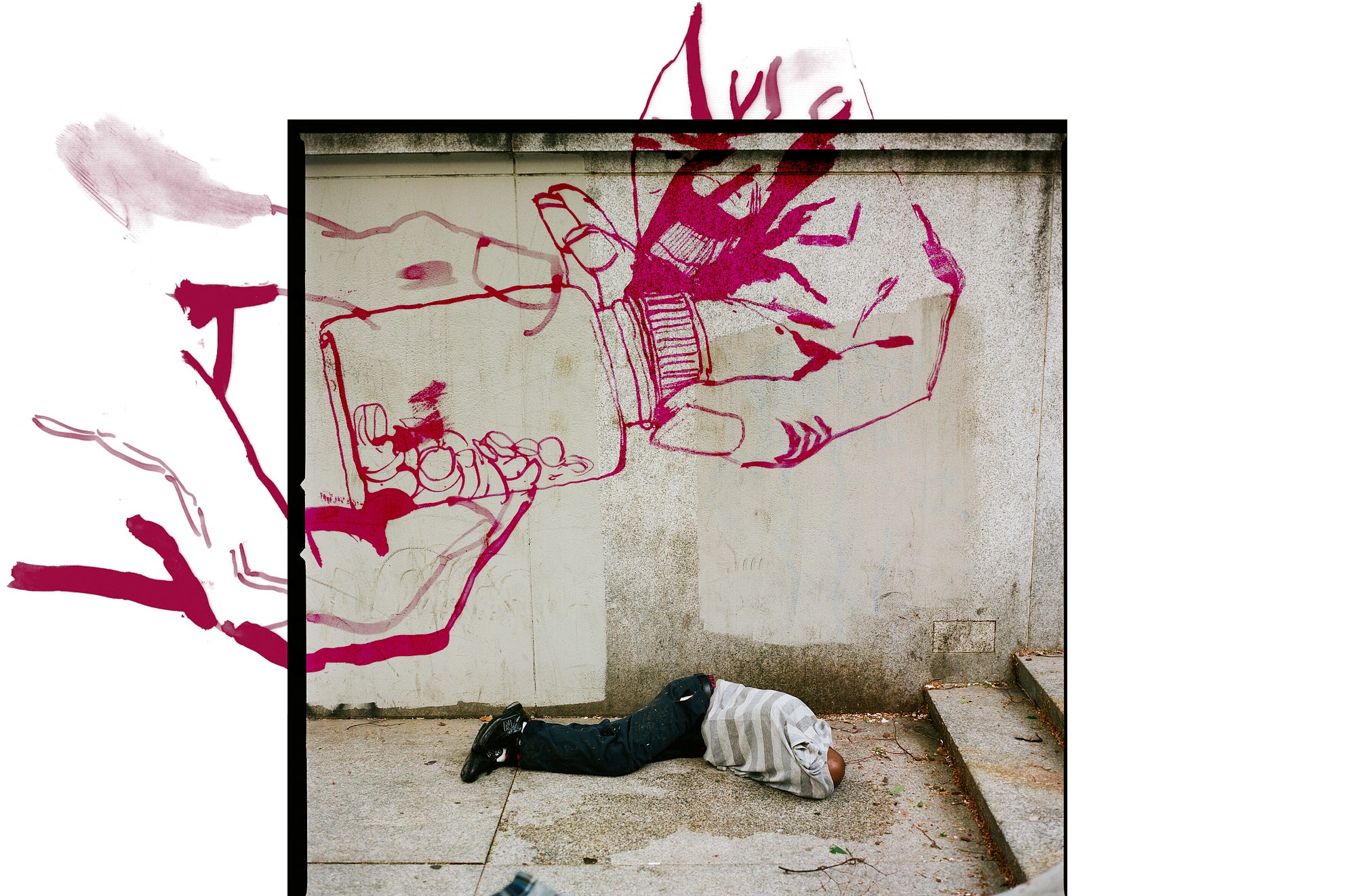
New types of drugs for schizophrenia, depression and other psychiatric disorders are few and far between—and a number of companies have scaled back or dropped development of this class of pharmaceuticals. One exception stands out. Ketamine, the anesthetic and illegal club drug, is now being repurposed as the first rapid-acting antidepressant drug and has been lauded as possibly the biggest advance in the treatment of depression in 50 years.
A few trials by large pharma outfits are now underway on a new, purportedly improved and, of course, more profitable variant of ketamine, which in its current generic drug form does not make pharmaceutical marketing departments salivate.
Some physicians have decided they simply can’t wait for the lengthy protocols of the drug approval process to be sorted out. They have read about experimental trials in which a low-dose, slow-infusion of ketamine seems to produce what no Prozac-like pill can achieve, lifting the black cloud in hours, not weeks.
With nothing to offer desperate, sometimes suicidal patients, physicians have decided against waiting for an expensive, ketamine lookalike to arrive and have started writing scripts for the plain, vanilla generic version that has been used for decades as an anesthetic. Ketamine, it seems, has captivated a bunch of white coats with the same grassroots energy that has propelled the medical marijuana movement.
No formal tally of off-label ketamine prescriptions has been made. But Carlos Zarate of the National Institute of Mental Health, a leader in researching ketamine for depression, receives numerous e-mails from physicians and patients. “It’s being used in many states,” Zarate says. “I know of [people in] California, New Jersey, Pennsylvania, New York, Texas Florida and around the world, Australia, Germany, the U.K.”
Physicians are allowed to prescribe drugs off-label—in other words, uses for which they have not received approval from a regulatory agency. The practice is widespread: in fact, ketamine itself is often administered for chronic pain, a use never approved by the U.S. Food and Drug Administration.
Legalities aside, not every physician thinks ketamine has met the required thresholds of safety and efficacy to become a mainstay of a walk-in clinic. “Clearly, the use of ketamine for treatment-resistant depression is not ready for prime time,” says Caleb Alexander, a physician who is a professor of epidemiology at Johns Hopkins University and co-director of the Johns Hopkins Center for Drug Safety and Effectiveness. “We have remarkably little solid scientific evidence to support its use in nonexperimental settings, that is to say, to support its use beyond research settings.”
Ketamine has a well-known side effect of inducing a trancelike state that club aesthetes dub the “K hole”—the reason it is known in clinical terminology as a “dissociative” anesthetic. Some users get sucked into the vortex spun by Special K, Vitamin K, “jet,” “special L.A. coke,” “K,” or one of the drug’s other monikers. The physician and neuroscientist John Lilly, known for his work on dolphin communication, almost drowned under the influence while immersed in his own invention, the sensory deprivation tank and had to resuscitated by his wife. Undeterred, Lilly continued binging, at one point injecting himself almost hourly for three weeks. Others haven’t been as lucky and have succumbed fatally to what Lilly’s wife called “the seduction of K.”
In the low doses administered in off-label clinics, side effects are rare or mild. “If I closed my eyes, images would present themselves like the opening credits of Dr. Who, with a tunnel of light,” says one patient.” Even so, a prospective patient must be carefully screened and turned away if there is any history of psychotic episodes.
In prescribing ketamine for depression, clinicians take it upon themselves to determine proper treatment protocols through trial and error, either by consulting colleagues or reading the methods sections of scientific papers that report the results of preliminary experimental trials not intended to evaluate the drug for clinical use. The risks are worth taking, say some psychiatrists, particularly if a patient has tried psychotherapy and one antidepressant after another with poor results—and any mention of electroconvulsive therapy produces a look of abject terror.
“I have patients who will try anything that is reasonably safe, says David Feifel, the physician who heads Adult Psychiatric Services at the University of California, San Diego, Medical Center. Feifel read the major study by Zarate in 2006 and decided to put in place one of the first clinical programs anywhere for ketamine therapy. After receiving approval from the hospital’s pharmacy and therapeutic committee, Feifel and his team began providing ketamine therapy on a routine basis in 2011. So far, 50 people with depression that did not respond to other treatments have been willing to pay out of pocket for the infusions. As many as three times that number, some from outside the U.S., have made inquiries.
Feifel shared some e-mails: “So many days I wake up and want to die, but not today,” wrote one patient after the therapy. “Thank you so much for this day of hope and contentment. It was the most beautiful day I can remember. I was a new person today and I’m looking forward to tomorrow, which is something I never say.” Another wrote: “I wanted to go out to eat last night and go for a walk today—both things I haven’t wanted to do for years.”
Feifel estimates that seven out of 10 patients have improved, a substantially higher number than respond to Prozac and other conventional antidepressants and a rate comparable to reports in experimental studies. Side effects have been minimal—and the high from the drug, no problem. “If anything, the patients enjoy that,” Feifel says.
Feifel does not see himself in the role of proselytizer. Whether ketamine becomes a depression breakthrough depends on overcoming treatment effects that often last just a few weeks, even with multiple infusions. “This is in my opinion the biggest challenge, whether this is really going be a game changer for depression or a limited tool is if we can figure out how to make this a durable benefit,” he says.
Feifel always lays out multiple treatment options tailored to a particular patient, not just ketamine alone. He might, for instance, try to disabuse patients of misconceptions about the dangers of electroconvulsive therapy. The hospital is also exploring other new approaches: transcranial magnetic stimulation, a magnetic field trained on a brain area affected by depression; and treatment with scopolamine, another anesthetic that may possibly offer patients quick mood relief.
Off-label prescribing of ketamine does not usually take place at major university hospitals like U.C. San Diego Medical Center but, rather, in small clinics, some of which appear to be largely devoted to dispensing the drug. “There’s nothing else they have to offer really,” Feifel says. That one-track approach has the drawback of possibly leaving a patient who doesn’t respond to ketamine feeling even more desperate.
* * * * *
By Gary Stix | September 12, 2013
Dennis Hartman, a 47-year-old former business executive for an Illinois gaming company, described the diagnosis he had been given as “major depression disorder with severity of the extreme, social phobia and generalized anxiety disorder,” something he had lived with for more than 30 years. He had tried Prozac-like drugs, an earlier generation of antidepressants, tranquilizers, mood stabilizers, supplements, meditation and psychotherapy. Nothing helped.
Last year he set a date and made a plan for how he would take his own life. He had given himself some time to get his affairs in order to cause as little distress as possible to his family. One night last fall before the date he had mentally set for himself, Hartman was up at 3 A.M., distraught and unable to sleep. Milling about the Web, he came upon an article about ketamine, an anesthetic and hallucinogenic club drug that is being intensively researched because of growing evidence that it can rapidly relieve major depression. He read about a study underway at the National Institutes of Health that was enrolling patients. He called the next day and was quickly accepted.
“I received a single infusion as part of that study,” Hartman says, “and I achieved 100 percent remission—a complete relief of all symptoms, which for me was dysphoria, anhedonia, extreme anxiety, cognitive impairment, very severe physical fatigue—I felt normal and healthy and happy within three or four hours after the infusion.”
The study protocol only allowed for one infusion—and the dramatic transformation began to gradually wear off beginning three weeks later. During that time Hartman, still at NIH as researchers conducted brain imaging and other studies, began a determined search of the Internet for a physician who might be willing to provide more ketamine, despite cautions conveyed by researchers that the drug was still experimental and had never been approved by the U.S. Food and Drug Administration for depression.
Hartman didn’t have far to look. Grassroots ketamine prescribing is on the upswing (read part 1), as physicians channel some of the same DIY-sentiment behind the medical marijuana movement, even while drug companies try to figure out ways to create a new class of antidepressant derived from ketamine’s chemical makeup. Ketamine itself holds little interest to pharma outfits because of its generic status. A raft of studies has shown that the compound can provide rapid reversal of symptoms for patients who have not responded to psychotherapy or the standard line of antidepressants.
Drugmakers have begun trials of ketaminelike pharmaceuticals. Some physicians, though, have decided that desperate patients simply can’t wait years for completion of clinical trials and regulatory approval. Prescribing a drug for a use other than the one for which it was approved—in other words, off the label—does not break any laws. That has given psychiatrists and anesthesiologists in the U.S. the latitude to begin prescribing ketamine from their offices or to set up small specialty clinics for dispensing the drug.
After he left the study Hartman went first to a physician in San Diego and later ended up at New York Ketamine Infusions in New York City where he received six treatments, at $525 apiece, which again achieved relief of the depression symptoms. Clinics like the one Hartman went to take their message to customers with direct, very direct, advertising. A drug company can get saddled with fines reaching into the megamillions if its sales reps promote a drug off-label. Nothing, however, stops a physician who prescribes off-label from buying an ad. Plugging ketamine resembles a cross between highway billboards trumpeting physicians offering Botox and drug company direct-to-consumer ads. The New York Ketamine Infusions Web site has a link titled: “Is Ketamine Right for me?” On the home page, the phrase “Dramatic Improvements in Mood within Hours flashes on the screen. A Massachusetts clinic offers a “revolutionary and promising new treatment” from a Dr. Ablow [first name omitted], identified on the site as “America’s most well-known psychiatrist.”
Acknowledging the amateurish marketing tone, Hartman says he will be “first in line” when the FDA approves a ketaminelike drug for depression, but for the moment the clinics are essential for him to deal with the profound anguish that has beset him his entire adult life. “When I’m talking to friends and family and people who have not heard my story, I try to make it an easy, brief metaphor,” he says. “I’m the guy in a burning car who is unconscious and there is somebody who could rescue me, and they have to smash out the window with a hammer or ax, and the people who are discouraging ketamine use are the ones who are saying: ‘Don’t hit that window because you might hit Dennis and you might hurt him.’ But if you don’t break the window with the ketamine ax, I’m going to die a horrible death. That’s how I view things.”
Physicians are treating more and more patients like Hartman. A Santa Barbara physician, Robert Early, had been interested for years in finding alternatives to electroconvulsive therapy for patients who didn’t respond or were petrified of the side effects. When a pivotal study on ketamine and depression was published in 2006, Early, then at Baylor College of Medicine in Houston, saw an opportunity and started doing the procedure within six months. There and in Santa Barbara, Early has administered the therapy to some 125 patients—having prescribed it more than 700 times to that group.
An Arizona entrepreneur may have the most ambitious vision for supplying ketamine: Gerald Gaines started a company last year called Depression Recovery Centers with a single clinic in Scottsdale. As the name suggests, Gaines wants to make a brand out of walk-in clinics for depression, perhaps expanding nationwide, making them as common as suburban kidney dialysis centers.
A Harvard MBA who was instrumental in the launch of Sprint PCS, Gaines has suffered from lifelong manic-depressive episodes—and has numerous family members who have also wrestled with depression. Gaines became involved with the medical marijuana business, with the hope that some of the multitude of compounds that can be isolated from the plant’s leaves might be extracted to help with mania. He still donates money for this line of research but has given up for the moment on the idea that a pot-derived depression drug will arrive anytime soon.
Instead, he became intrigued with research on ketamine, which led to his opening the Scottsdale clinic. So far, the clinic has treated 30 patients under the care of an anesthesiologist and a psychologist. Most patients require more than one infusion, and the clinic has delivered in excess of 200 infusions since it opened. (The clinic posted “Tiffany’s Transformation Day” on Vimeo about one patient’s before-and-after experience.) Gaines himself is a customer. “I’ve been symptomatic for 45 years and have had two or three depressions every year, except for the last year, when I’ve had none,” he says. “I’ve had five treatments in last 12 months, and that’s the typical pattern of what we’re seeing for bipolar disorder.”
The cost of each infusion, at $750, is not covered by insurance. “Our target market very unfortunately—anybody who knows me knows I don’t feel good about this—is the top 10 percent of family income individuals,” Gaines says. A course of treatment typically costs $4,000 and can range up to $15,000—and may need to be repeated as the effects wear off.
Absent large-scale clinical trials, ketamine for depression will remain a form of drug development based on testimonial and anecdote. Drugs in the pipeline at major pharmaceutical companies may help fill in some of the blanks, but the first one may not arrive before 2017 and questions linger about whether these rejigged versions of ketamine will be any better than what is currently available from off-label clinics.
* * * * *
By Gary Stix | September 13, 2013

Ketamine induces growth of tiny protuberances on a rat neuron (bottom)
to allow it to better connect with neighbors.
Recent experimental research showing that the anesthetic and club drug ketamine can relieve depression quickly has intrigued a number of major pharmaceutical companies. Depression, it goes without saying, affects huge numbers and a fundamentally new and effective pharmaceutical approach to treating the disorder hasn’t emerged in decades.
The enthusiasm for ketamine is such that physicians, often working out of small clinics, have already started prescribing low doses of the generic anesthetic off-label for fast relief of le cafard—and drug companies are contemplating whether to get into the act by creating new drugs based on ketamine’s biochemistry (Read part 1 and part 2).
A Johnson & Johnson subsidiary in Europe has gone as far as midstage clinical trials for a ketamine nasal spray. The trial there uses a slightly altered version of ketamine (esketamine, the “s” isomer for techies), which omits part of the molecule and leaves the most pharmacologically active portion in place, enabling less of the compound to be administered. “You can get away with a 30 to 40 percent lower dose,” says Husseini Manji who leads neuroscience research at Johnson & Johnson.
The U.S. Food and Drug Administration has put Johnson & Johnson’s version of esketamine on a fast track for approval, although, even if all goes well, patients may still have to wait a years to get a script. Esketamine, already used as an anesthetic in Europe, is not the only idea on the table. Ketamine appears to work (details still coming in from labs) by blocking a docking site, or receptor, on a neuron—in this case a spot where the essential signaling molecule glutamate attaches. The blockade triggers a complex chemical cascade that ends up restoring an impaired neuron’s ability to communicate with other brain cells.
If that process is multiplied over millions of neurons in two critical brain regions—the hippocampus and the prefrontal cortex—drugmakers hope the blues will lift like a cloud. Johnson & Johnson is working on other projects that tap into ketamine research—one of which is looking at a wholly new drug that targets selected portions of this glutamate receptor in the hope of fine-tuning the antidepressant effects further. Other large pharmas, including AstraZeneca and Roche, are pursuing similar strategies.
If a formal FDA imprimatur is forthcoming, the issue of off-label prescribing may persist. One issue, which must be resolved through clinical trials rather than trial and error at ketamine clinics, is whether a spray works as well as intravenous infusions. The generic non-isomer form of ketamine is already used off-label as a nasal spray and not all reviews are positive. “It helped but not as much as the infusion,” says Dennis Hartman, a patient with depression who sought help from ketamine-prescribing physicians, one of whom provided a spray.
A ketamine-like drug, if approved, will inevitably be more expensive than the generic anesthetic deployed in upstart depression clinics. Esketamine or one of its FDA-sanctioned cousins will probably be covered via a health insurance plan, but insurers’ love of low-cost generics may mean that consideration could still be given to covering plain-vanilla ketamine, even if it hasn’t run the clinical-trial gantlet. In fact, Carlos Zarate, a leading ketamine researcher who works at the National Institute of Mental Health, has even fielded calls from insurers wanting to know more about the generic drug to determine whether to put it on their formularies.
It is also still unclear whether the medical establishment, with a helping hand from law enforcement, may have to come to terms with what might be described as off–off-label prescribing—the depressed patient without insurance who learns about the possibility of a mood-altering quick fix and engages in the unsupervised self administration of Special K purchased in a club or on the street.
Hartman knows someone who went this route. “This personal friend received a ketamine infusion [from a physician],” Hartman says. “He achieved very strong relief, very similar to mine. After he relapsed, he went and sought this illegal form and he did not get the same effect.” If Johnson & Johnson’s esketamine trials result in a salable drug, the company has plans to safeguard it from those who want to divert it for recreational use.
What to do about ketamine is a question being posed everywhere, not just stateside. A New Zealand government official issued a report in July that instructed health boards throughout the country to scrutinize off-label prescribing more closely after a complaint lodged against a ketamine-supplying physician.
Inevitably, the grassroots appeal of an old drug with a new use that might provide hope for the deeply depressed is starting to generate its own social networks. As many as 20 physicians involved in prescribing ketamine interact on the Linked-In group called Ketamine for Psychiatry. Hartman is involved with setting up a new Web site, The Ketamine Advocacy Network, to foster activism among patients—another echo of medical marijuana’s legacy.
The desperation to find new antidepressants means that ketamine will remain an object of fascination for mental health professionals and their patients. In the next five years, regulators and physicians are going to have to figure out how, if at all, the drug fits into the psychiatrist’s pharmacopoeia. In the meantime, doctors and patients are increasingly adopting their own home-grown solutions.
About the Author: Gary Stix, a senior editor, commissions, writes, and edits features, news articles and Web blogs for SCIENTIFIC AMERICAN. His area of coverage is neuroscience. He also has frequently been the issue or section editor for special issues or reports on topics ranging from nanotechnology to obesity. He has worked for more than 20 years at SCIENTIFIC AMERICAN, following three years as a science journalist at IEEE Spectrum, the flagship publication for the Institute of Electrical and Electronics Engineers. He has an undergraduate degree in journalism from New York University. With his wife, Miriam Lacob, he wrote a general primer on technology called Who Gives a Gigabyte? Follow on Twitter @@gstix1.
The views expressed are those of the author and are not necessarily those of Scientific American.

 Research advances medicine but conflicts of interest can corrupt outcomes and compromise patient care. (Photo credit: Wikipedia)
Research advances medicine but conflicts of interest can corrupt outcomes and compromise patient care. (Photo credit: Wikipedia)