Lewis is the author of Memoirs of an Addicted Brain: A Neuroscientist Examines his Former Life on Drugs and co-editor of Emotion, Development, and Self-Organization: Dynamic Systems Approaches to Emotional Development.
Brain patterns formed by trauma sometimes need fixing—at any price
A while back I promised to survey the three most common models of addiction—disease, choice, and self-medication—and say something about the advantages and disadvantages of each. I got hung up on the choice model for a few posts: there’s so much there to think about. But now let’s look at self-medication as the essence of addiction.
The self-medication model seems to be the kindest of the three. It has the advantage of the disease model, in absolving the addict of excessive blame, but it has the additional advantage of avoiding the stigma of “disease” and all that goes with it. In fact, it gives control (agency) back to the addict, who is, after all, acting as his or her own physician. Whereas the disease model places agency in the hands of others and casts the addict as a passive victim. Furthermore, the self-medication model just might be the most accurate of the three.
The idea is simple: trauma is the root cause. Trauma includes abuse, neglect, medical emergencies, and other familiar categories, but it also includes emotional abuse, and above all loss. Loss of a parent during childhood or adolescence can take many forms, including divorce, being sent away from home (in my case) or the shutting down of one or both parents due to depression or other psychiatric problems. Trauma is often followed by post-traumatic stress disorder (PTSD), which includes partial memory loss, intrusive thoughts, anxiety and panic attacks, avoidance of particular places, people, or contexts, emotional numbing or a sense of deadness, and overwhelming feelings of guilt or shame. But if that’s not bad enough, PTSD is about 80% comorbid with other psychiatric conditions—depression and anxiety disorders being chief among them.
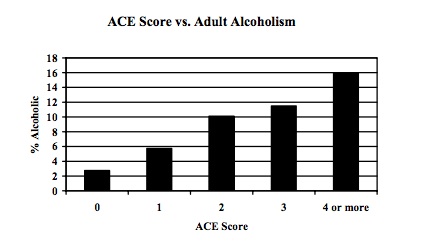
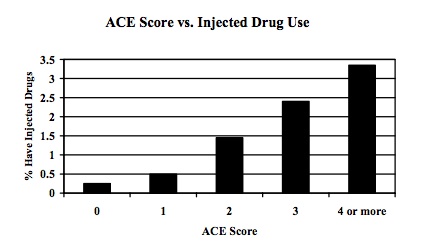
A famous study using a huge sample (17,000) looked at Adverse Childhood Experiences (ACEs) in relation to subsequent physical and mental problems. The results of the study are nicely summarized in the Sept. 25/2011 issue of The Fix. Take-home message: the relationship between trauma and addiction is unquestionable. An ACE score was calculated for each participant, based on the number of types of adverse experience they reported during childhood or adolescence. The higher the ACE score, the more likely people were to end up an alcoholic, drug-user, food-addict, or smoker (among other things). Here are two graphic examples:
These figures, which are likely to be low estimates, show a 500% increase in the incidence of adult alcoholism, and a 4,600% increase in the incidence of IV drug use, predicted by early adverse experiences. Despite criticisms of the study, based mostly on retrospective self-reporting, these correlations are huge and they are meaningful, and follow-up prospective studies are finding similar results.
So how does self-medication work? There must be something about PTSD, depression, and anxiety that gets soothed by drugs, booze, binge-eating, and other addictive hobbies. Again, it’s not complicated. PTSD, depression, and anxiety disorders all hinge on an overactive amygdala—one that is not controlled or “re-oriented” by more sophisticated (and realistic) appraisals coming from the prefrontal cortex and anterior cingulate cortex (ACC). That traumatized amygdala keeps signalling the likelihood of harm, threat, rejection, or disapproval, even when there is nothing in the environment of immediate concern. In fact, this gyrating amygdala lassos the prefrontal cortex, foisting its interpretation on the orbitofrontal cortex (and ventral ACC) rather than the other way around (which we might loosely call emotion regulation). The whole brain is dominated by limbic imperialism—making it a less-than-optimal neighbourhood in which to reside.
At the very least, drugs, booze, gambling and so forth take you out of yourself. They focus your attention elsewhere. They may rev up your excitement and anticipation of reward (in the case of speed, coke, or gambling) or they may quell anxiety directly by lowering amygdala activation (in the case of downers, opiates, booze, and maybe food). The mechanisms by which this happens are various and complex. But addicts and ex-addicts (like me) know what it feels like. If we find something that relieves the gnawing sense of wrongness, we take it, we do it, and then we do it again.
So, according to the self-medication model, addictive behaviours “medicate” depression, anxiety, and related feelings. But is that the whole story? I don’t think so, and I’ll get into why in my next post.

No comments:
Post a Comment