
The title of this talk is the nearly identical to that of a new book from Bessel van der Kolk due out in June, 2014 - The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma (pre-order at Amazon). I will be excited to see this new work - his research in the recent years has focused on yoga, tapping (Emotional Freedom Technique), chi gong, and neurofeedback, among other body-centered modalities for healing trauma.
What follows are my notes, as best as I can make them sensible from today's 3 hour talk.This is part one - part two will follow soon.
The Body Keeps the Score
In the 1920s, Pavlov's lab was flooded and his dogs ended up standing in cold water for two days before being "rescued." During this time they were in their cages, unable to flee. Pavlov assessed that they were flooded with stress hormones during that time, but they were not able to metabolize them as a result of being caged - they could not fight or flee. His notes on this reveal with physiological impact of unresolved trauma - a definition that remained until the DSM system was created and the trauma response "became" psychological. Until the DSM, trauma was always conceptualized in the body.
BvdK showed some video clips of WWI soldiers with "shell-shock" - man who shot the enemy soldier in the face and now has a compulsive facial tick; a man who lost all function of his limbs after surviving an explosion and years later still could barely walk; a man who was unable to pick himself up off of the floor in the absence of any physical injury. These are examples of how the body re-enacts the trauma, of automatic responses completely outside of conscious control or willpower.
One of many asides on the inadequacy of cognitive behavioral therapy (CBT) for the treatment of trauma (there are a lot of CBT experts here who talk about all the ways to work verbally with trauma, while not understanding that trauma is not a verbal experience - more on this idea below):
CBT is misguided in treating trauma because when the trauma system gets activated, the prefrontal cortex (executive function) goes offline and the limbic system is running the show. CBT works with executive function, not with the body-based emotions encoded by the limbic system.
Even when trauma is long past, it replays itself in the body through pain, anxiety, depression, illness, digestive issues, and so on. We must help the client learn to tolerate the physiological trauma symptoms while remaining in their bodies - since nearly all PTSD is dissociative in some way.
Sleep: Trauma survivors wake themselves from REM sleep when their dreams contain images or scenes or sensations of their trauma. REM sleep is designed to allow us to integrate learning and experience while we sleep, but this gets short-circuited in trauma. The ability to dream may be the best indicator of resilience in survivors.
EMDR is not a verbal therapy, it ignores the linguistic narrative. EMDR works via the anterior cingulate, a brain region responsible for distinguishing past from present, safe from dangerous, or relevant from not relevant, among others. It works with the "that was then, this is now" function of the brain - verbal/talk therapies cannot access this brain module. --- Acute single episode trauma can often be resolved in 6-8 sessions using EMDR. At the end of a successful EMDR treatment for a single-episode trauma, the survivor will be able to tell the story with no emotional overwhelm or activation.
James W. Pennebaker says that if people can write about (journaling) the worst details of their worst experience(s), 15 minutes a day, every day for 4 consecutive days, their lives can improve considerably. This process helps them to know what they know and feel what they feel. Telling themselves the story, confirming their own experience, is much more effective than telling someone else the story. --- The reason for this is that feeling the internal world lights up one part of the brain (medial prefrontal cortex) and talking about that experience lights up another part of the brain (dorsolateral prefrontal cortex, home of Broca's Area). These two parts of the brain are only tenuously connected.
Fight/Flight/Freeze/Fold
All four trauma responses activate the body's stress response system, BUT . . . .
- In fight and flight, the stress hormones get used in the act of fighting or running away. These responses generally do not develop PTSD in a single episode trauma (assuming no trauma history).
- In freeze and fold, all of the stress hormones are released, but they are not metabolized through physical action because the individual freezes or essentially goes limp in surrender. These people are very likely to develop PTSD because the stress response was not discharged and becomes stuck in the body/mind.
For example, following 9/11 in NYC, citizens banded together and supported each other, not to mention being supported by the nation and people around the world. The most traumatized people were the first responders and rescue workers, and then some of the survivors - but the city itself was not overly traumatized.
On the other hand, with Hurricane Katrina in New Orleans, people were stuck on the roofs of their homes, unable to escape the water, or herded into the Super Dome, which was dark, leaked, and filthy (remember Pavlov's dogs), or prevented from crossing a bridge out of the city. More than 33% of the people in N.O. suffered from PTSD.
In PTSD, the body's instinct to fight or flee is stifled and it freezes (often connected with forms of dissociation) or folds, simply gives up and seemingly says, "take me, I won't resist." These avoidance tactics are not healthy in the long-term, even though they may be the only option in the moment. Survivors in this mode are flooded with all of the same stress hormones again any time they remember or re-experience some aspect of the trauma.
If there was pain involved in the original event, whether it was childhood molestation or being thrown violently from a horse, the body releases opiates to squash the pain. But when we relive the event, the same chemicals are released and in the absence of pain the person feels nausea. I cannot count the number of times a client has said, "I feel sick," referring to nausea when reliving or retelling a traumatic experience that reactivates the limbic system.
Vagus Nerve
Charles Darwin identified the vagus nerve (cranial nerve X) in 1872. He recognized its connection to and central role in expressing and managing emotions. When the mind is strongly activated, the body is immediately affected, and the arousal information is relayed by the vagus nerve.
[Side note: Nearly impossible to be an addict without a trauma history - addiction is a way to manage (self-medicate) intense and overwhelming emotions in the body.]
Stephen Porges is the person who has done the most to bring the physiological facts of the role of the vagus nerve in trauma into the world of trauma treatment.
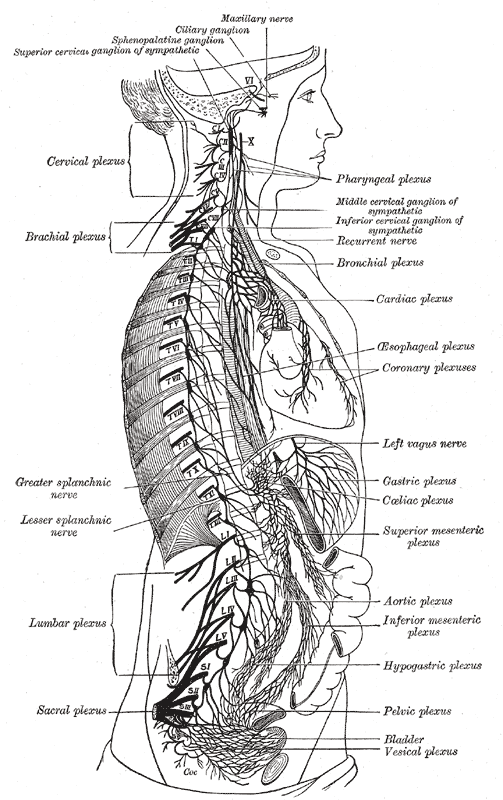
In the vagus, 80% of the fibers are afferent, meaning they carry information to the central nervous system (brain). Here's more from Health Line:
It extends from the brain stem to the abdomen, via various organs including the heart, esophagus and lungs. Also known as cranial nerve X, the vagus forms part of the involuntary nervous system and commands unconscious body procedures, such as keeping the heart rate constant and controlling food digestion.The vagus is also responsible for many of the nerves in the mouth, including speech.

Consistent and considerable research has shown that body posture has a LOT to do with affect states and can shape our emotions. Slumping our shoulders forward and looking down at the ground supports and maintains a depressed attitude physiologically and psychologically.
One of the "positive psychology" interventions is to smile even when we are sad, or to laugh when we are depressed. Doing so can shift brain chemicals toward those supporting health and away from those supporting dis-ease.
Finally, depression, joylessness lack of purpose, and so on are all sourced in our disconnection from the body. We disconnect from the body to avoid our pain, our trauma, but in doing so we also lose the body's vitality and passion, and we become depressed.
Go on to part two.
No comments:
Post a Comment