Weak Brain Connections Found in People with Anxiety Disorder
Reviewed by John M. Grohol, Psy.D. on September 5, 2012The brains of people with generalized anxiety disorder (GAD) have weaker connections between a brain region in charge of emotional response and the amygdala.
This suggests that the brain’s “panic button” may be chronically pushed down due to lack of regulation, according to a new University of Wisconsin-Madison imaging study.
GAD, which is characterized by excessive, uncontrollable worry, affects nearly 6 percent of the population.
The findings support the hypothesis that reduced communications between parts of the brain result in the extreme anxiety felt by people with GAD, said lead author Jack Nitschke, Ph.D., associate professor of psychiatry.
* * * * *
Neuroscience: Idle minds
Neuroscientists are trying to work out why the brain does so much when it seems to be doing nothing at all.For volunteers, a brain-scanning experiment can be pretty demanding. Researchers generally ask participants to do something — solve mathematics problems, search a scene for faces or think about their favoured political leaders — while their brains are being imaged.
But over the past few years, some researchers have been adding a bit of down time to their study protocols. While subjects are still lying in the functional magnetic resonance imaging (fMRI) scanners, the researchers ask them to try to empty their minds. The aim is to find out what happens when the brain simply idles. And the answer is: quite a lot.
Some circuits must remain active; they control automatic functions such as breathing and heart rate. But much of the rest of the brain continues to chug away as the mind naturally wanders through grocery lists, rehashes conversations and just generally daydreams. This activity has been dubbed the resting state. And neuroscientists have seen evidence that the networks it engages look a lot like those that are active during tasks.
Resting-state activity is important, if the amount of energy devoted to it is any indication. Blood flow to the brain during rest is typically just 5–10% lower than during task-based experiments1. And studying the brain at rest should help to show how the active brain works. Research on resting-state networks is helping to map the brain's intrinsic connections by showing, for example, which areas of the brain prefer to talk to which other areas, and how those patterns might differ in disease.
But what is all this activity for? Ask neuroscientists — even those who study the resting state — and many will sigh or shrug. “We're really at the very beginning. It's mostly hypotheses,” says Amir Shmuel, a brain-imaging specialist at McGill University in Montreal, Canada. Resting activity might be keeping the brain's connections running when they are not in use. Or it could be helping to prime the brain to respond to future stimuli, or to maintain relationships between areas that often work together to perform tasks. It may even consolidate memories or information absorbed during normal activity.
* * * * *
Beyond the Brain
In the 1990s, scientists declared that schizophrenia and other psychiatric illnesses were pure brain disorders that would eventually yield to drugs. Now they are recognizing that social factors are among the causes, and must be part of the cure.By the time I met her, Susan was a success story. She was a student at the local community college. She had her own apartment, and she kept it in reasonable shape. She did not drink, at least not much, and she did not use drugs, if you did not count marijuana. She was a big, imposing black woman who defended herself aggressively on the street, but she had not been jailed for years. All this was striking because Susan clearly met criteria for a diagnosis of schizophrenia, the most severe and debilitating of psychiatric disorders. She thought that people listened to her through the heating pipes in her apartment. She heard them muttering mean remarks. Sometimes she thought she was part of a government experiment that was beaming rays on black people, a kind of technological Tuskegee. She felt those rays pressing down so hard on her head that it hurt. Yet she had not been hospitalized since she got her own apartment, even though she took no medication and saw no psychiatrists. That apartment was the most effective antipsychotic she had ever taken.
Twenty years ago, most psychiatrists would have agreed that Susan had a brain disorder for which the only reasonable treatment was medication. They had learned to reject the old psychoanalytic ideas about schizophrenia, and for good reasons. When psychoanalysis dominated American psychiatry, in the mid-20th century, clinicians believed that this terrible illness, with its characteristic combination of hallucinations (usually auditory), delusions, and deterioration in work and social life, arose from the patient’s own emotional conflict. Such patients were unable to reconcile their intense longing for intimacy with their fear of closeness. The science mostly blamed the mother. She was “schizophrenogenic.” She delivered conflicting messages of hope and rejection, and her ambivalence drove her child, unable to know what was real, into the paralyzed world of madness. It became standard practice in American psychiatry to regard the mother as the cause of the child’s psychosis, and standard practice to treat schizophrenia with psychoanalysis to counteract her grim influence. The standard practice often failed.
The 1980s saw a revolution in psychiatric science, and it brought enormous excitement about what the new biomedical approach to serious psychiatric illness could offer to patients like Susan. To signal how much psychiatry had changed since its tweedy psychoanalytic days, the National Institute of Mental Health designated the 1990s as the “decade of the brain.” Psychoanalysis and even psychotherapy were said to be on their way out. Psychiatry would focus on real disease, and psychiatric researchers would pinpoint the biochemical causes of illness and neatly design drugs to target them.
Schizophrenia became a poster child for the new approach, for it was the illness the psychoanalysis of the previous era had most spectacularly failed to cure. Psychiatrists came to see the assignment of blame to the schizophrenogenic mother as an unforgivable sin. Such mothers, they realized, had not only been forced to struggle with losing a child to madness, but with the self-denigration and doubt that came from being told that they had caused the misery in the first place. The pain of this mistake still reverberates through the profession. In psychiatry it is now considered not only incorrect but morally wrong to see the parents as responsible for their child’s illness. I remember talking to a young psychiatrist in the late 1990s, back when I was doing an anthropological study of psychiatric training. I asked him what he would want non-psychiatrists to know about psychiatry. “Tell them,” he said, “that schizophrenia is no one’s fault.”
It is now clear that the simple biomedical approach to serious psychiatric illnesses has failed in turn. At least, the bold dream that these maladies would be understood as brain disorders with clearly identifiable genetic causes and clear, targeted pharmacological interventions (what some researchers call the bio-bio-bio model, for brain lesion, genetic cause, and pharmacological cure) has faded into the mist. To be sure, it would be too strong to say that we should no longer think of schizophrenia as a brain disease. One often has a profound sense, when confronted with a person diagnosed with schizophrenia, that something has gone badly wrong with the brain.
* * * * *
The Creativity of the Wandering Mind
New research suggests engaging in simple tasks that allow the mind to wander facilitates creative thinking.
Do you have a numbingly dull job, one so monotonous that you frequently find your mind wandering? Well, congratulations: without realizing it, you have boosted your creative potential.
Mindless tasks that allow our thoughts to roam can be catalysts for innovation. That’s the conclusion of a research team led by Benjamin Baird and Jonathan Schooler of the University of California, Santa Barbara’s META Lab (which focuses on Memory, Emotion, Thought and Awareness).
Their research, published in the journal Psychological Science, suggests putting a difficult problem in the back of your mind won’t, by itself, lead to creative thinking. The key seems to be performing some simple chore while it’s lodged there.
Baird and his colleagues describe an experiment featuring 135 people, ages 19 to 35. Their creativity was measured by performance on the classic Unusual Uses Task, in which each participant is given two minutes to come up with as many uses as possible for a specific item, such as a brick. Besides the sheer number of responses, their answers are judged on originality, flexibility, and level of detail.
All the participants began by tackling two such problems. One-quarter of them then spent 12 minutes on an intellectually demanding task, which demanded constant attention. Another quarter spent that same amount of time on an undemanding task, which only required them to provide “infrequent responses.” Another quarter was instructed to rest for 12 minutes, while the rest went directly to the next task without a break.
All then tackled four additional rounds of the Unusual Uses Task. Two were repeats of the tests they performed earlier, and two featured objects that were new to them.
Those who had performed the undemanding task in the interim had significantly higher scores than those in any of the other categories (including the people who had simply rested for 12 minutes). However, this jump in creativity occurred only for the items they were tackling for a second time. They did not score any better than the others when presented with a new object.
This suggests their success in coming up with creative solutions “resulted from an incubation process” which was “characterized by high levels of mind wandering,” the researchers write.
* * * * *
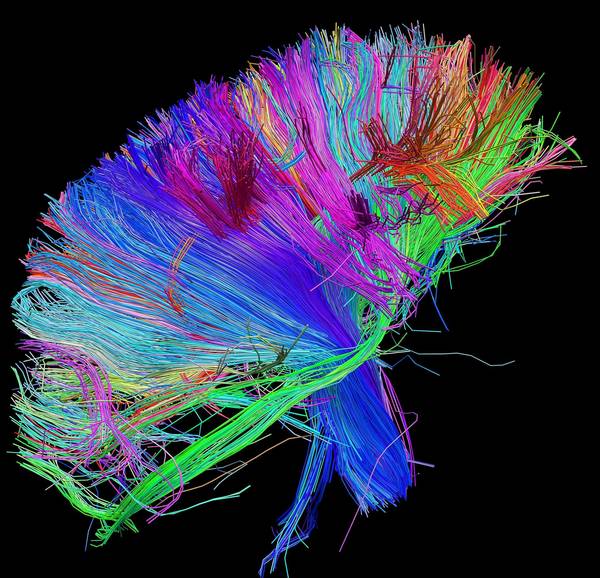
Neuroscience mapping brain connections
Discoveries could yield an understanding of and treatments for disorders such as autism, schizophrenia, depression and Parkinson's disease.
Inside the human skull lies a 3-pound mystery. The brain — a command center composed of tens of billions of branching neurons — controls who we are, what we do and how we feel.
"It's the most amazing information structure anybody has ever been able to imagine," says Dr. Walter Koroshetz, deputy director of the National Institute of Neurological Disorders and Stroke in Bethesda, Md.
For centuries, the brain's inner workings remained largely unexplored. But all that is changing. With the help of new tools, researchers are delving deeper into this complex organ than ever before. We're in a brainy age of discovery that could change our understanding of how the brain works and why, in some cases, it fails to do its job.
Scientists already have an intimate knowledge of brain anatomy, from the hippocampus to the amygdala. "We've mapped these in exquisite detail," says Arthur Toga, director of the Laboratory of Neuro Imaging at UCLA.
But those maps don't show how the regions connect. And it's this connectivity that enables the complex behaviors our brains perform so seamlessly.

No comments:
Post a Comment