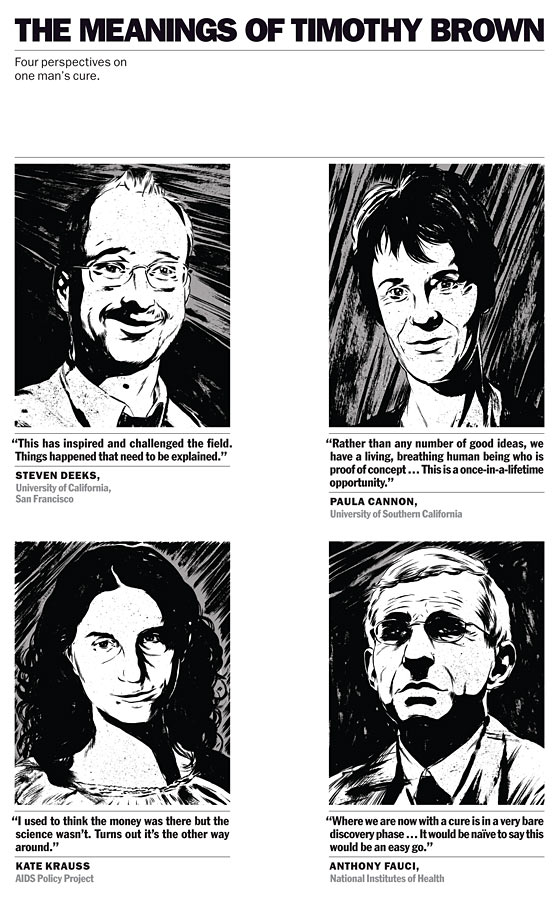
The Man Who Had HIV and Now Does Not
Four years ago, Timothy Brown underwent an innovative procedure. Since then, test after test has found absolutely no trace of the virus in his body. The bigger miracle, though, is how his case has experts again believing they just might find a cure for AIDS.
AIDS is a disease of staggering numbers, of tragically recursive devastation. Since the first diagnosis, 30 years ago this June 5, HIV has infected more than 60 million people, around 30 million of whom have died. For another 5 million, anti-retroviral therapy has made their infection a manageable though still chronic condition. Until four years ago, Timothy Brown was one of those people.
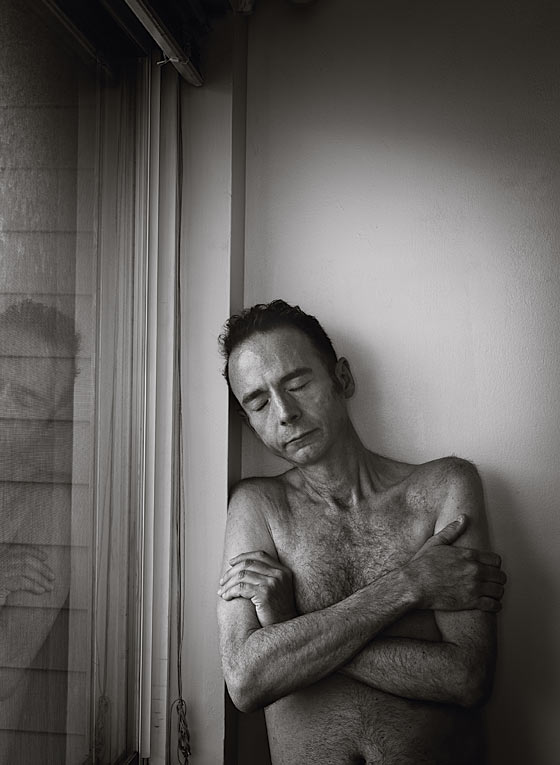
Brown is a 45-year-old translator of German who lives in San Francisco. He is of medium height and very skinny, with thinning brown hair. He found out he had HIV in 1995. He had not been tested for the virus in half a decade, but that year a former partner turned up positive. “You’ve probably got only two years to live,” the former partner told him when Brown got his results.
His partner was wrong—lifesaving anti-retrovirals were about to arrive—and Brown spent the next ten years living in Berlin, pursuing his career and enjoying the city by night. He was gregarious, a fast talker; when he went out, he’d always wind up the center of a group. “I used to be quite a flirt,” he tells me. “I would see someone in a café, bar, or disco and knew how to get what I wanted.” In 2006, Brown was living in Berlin with his boyfriend, a man named Michael from the former East Germany. That year, on a trip to New York for a wedding, he began to feel miserable. He chalked it up to jet lag, but it didn’t go away. Back in Berlin, his bike ride to work took so long that he got chewed out by his boss for lateness. Michael called his doctor, who saw Brown the next day.
The results came back: leukemia. A new, unrelated disease was now threatening his life. Michael cried. Brown was referred to Charité Medical University, where he was treated by Gero Hütter, a 37-year-old specialist in blood cancers.
After chemo, the leukemia came back. Brown’s last chance was a stem-cell transplant from a bone-marrow donor. Hütter had an idea. He knew little about HIV, but he remembered that people with a certain natural genetic mutation are very resistant to the virus. The mutation, called delta 32, disables CCR5, a receptor on the surface of immune-system cells that, in the vast majority of cases, is HIV’s path inside. People with copies from both parents are almost completely protected from getting HIV, and they are relatively common in northern Europe—among Germans, the rate is about one in a hundred. Hütter resolved to see if he could use a stem-cell donor with the delta-32 mutation to cure not just Brown’s leukemia but also his HIV.
Hütter found 232 donors worldwide who were matches for Brown. If probabilities held, two would have double delta 32. Hütter persuaded the people at the registry to test the donors for the mutation; his laboratory paid, at a cost of about $40 per sample. They worked through the list. Donor 61 was a hit.
His colleagues and the chief of his unit were dubious. “The main problem was that I was just a normal physician—I had no leading position. It was not always easy to get what we needed,” Hütter recalls. Brown himself was not pushing the idea. “At that point, I wasn’t that concerned about HIV, because I could keep taking medication,” he says.
Before Hütter asked the donor registry to begin testing, he’d searched the literature and contacted AIDS experts. It dawned on him that no one had ever done this before. “My first thought was, I’m wrong. There must be something I was missing.” In a sense, that was true. Gero Hütter did not know what most AIDS researchers and clinicians had taken as accepted wisdom: A cure was impossible.
The 1996 International Conference on AIDS in Vancouver brought the stunning announcement that a combination of three anti-retroviral drugs could keep HIV in check. David Ho, director of New York’s Aaron Diamond AIDS Research Center, went further. In the closing session, Ho said that it might be possible to eradicate the disease from the body with 18 to 36 months of therapy. Time magazine named Ho “Man of the Year.”
But Ho was too optimistic. Treatment with the drugs, no matter how early it’s begun, cannot eradicate HIV, because the virus hides, lurking in the brain or liver or gut without replicating, invisible to the immune system. It is waiting to come roaring back if therapy is stopped. Disillusioned, some cure researchers transferred their finite resources and energy to improving AIDS treatment or working on a vaccine. Money for cure research dried up. Some scientists took to calling it “the C-word” or “cure” with air quotes.
Meanwhile, advances in treatment have further shifted attention from the hunt for a cure. A study released in May found that early anti-retroviral therapy decreases patients’ infectiousness by a striking 96 percent. Today, most people on anti-retroviral drugs achieve an undetectable viral load—there is virtually no HIV circulating in their blood. An idea has taken hold: We can live with this.
But we cannot. Doctors will tell you that many patients still fail treatment and die. As people age with the disease, we are seeing that even those successfully treated can lose years of life. A massive multicountry study published in The Lancet in 2008 reported that someone starting therapy at age 20 could expect to live to only 63. The following year, another study found that a group of HIV-positive patients with a median age of 56 had immune systems comparable to those of healthy 88-year-olds. The latent reservoir of HIV seems to be most to blame, producing inflammation that degrades the immune system, increasing susceptibility to age-related diseases. What’s more, research has shown that the drugs themselves can lead to increased risk of heart disease, diabetes, and osteoporosis.
The cost of treatment is also unsustainable. In the United States, second-line drugs—for people who don’t improve on standard medications—can total $30,000 a year. Cash-strapped states are trimming programs that pay for these medicines; there are now more than 8,300 people in America on waiting lists for anti-retroviral drugs. In developing countries, drugs are much cheaper—some generic regimens cost only $67 annually—but wealthy nations are wearying of picking up the bill. According to UNAIDS, 10 million people in the Third World who need treatment are not getting it at all. The math of the epidemic is unrelenting: For every three people who start treatment, five new people are infected.
A vaccine for AIDS is “probably decades away,” says Daria Hazuda, a vice-president at Merck. “There’s still an enormous amount of hope, but people now realize it’s going to be extremely complicated.” We know now that we will neither treat nor vaccinate our way out of this epidemic. But there could be another way for it to end.
In February 2007, Brown had his stem-cell transplant from Donor 61. Right before the procedure, he stopped taking his anti-retrovirals. He survived the operation—no small feat, since stem-cell transplants from unrelated donors kill a hefty minority of the people who undergo them. His initial recovery was encouraging. “I went back to work, started working out at a gym and riding my bicycle again,” he says.
Then Brown relapsed. In February 2008, Hütter did another transplant from Donor 61. (Going back to the same donor is standard; the patient is now accustomed to that immune system.) This time, the cancer seems to have stayed away. More striking: More than four years after he stopped taking anti-retroviral therapy, there is also no sign of HIV in his body. Brown is now surely one of the most biopsied humans on Earth. Samples from his blood, his brain, his liver, his rectum, have been tested over and over. People in whom the disease is controlled with anti-retroviral therapy will still have hidden HIV—perhaps a million copies. But with Brown, even the most sensitive tests detect no virus at all. Even if trace amounts remain (it is impossible to test every cell), it no longer matters. Absent the CCR5 receptors, any HIV still present cannot take root. He is cured.
A stem-cell transplant from an unrelated donor can cost $250,000 and is a reasonable risk only in the face of imminent death. What cured Timothy Brown is obviously not a cure for the rest of the world. But it is proof of concept, and it has jolted AIDS-cure research back to life. Sometimes science follows sentiment; the abandonment of cure research after the disillusion of the nineties is now playing out in reverse.
For Brown’s cure to be relevant on a wide scale, it would have to be possible to create the delta 32 mutation without a donor and without a transplant—preferably in the form of a single injection. As it happens, progress toward that goal has already begun, in the laboratory of Paula Cannon at the University of Southern California. Instead of a donor, Cannon is using a new form of gene editing known as zinc finger nucleases, developed by the California company Sangamo BioSciences. Zinc finger nucleases are synthetic proteins that act as genetic scissors. They can target and snip a specific part of the genetic blueprint: They can, for instance, cut out the code that produces the CCR5 receptor, yielding a cell with HIV resistance.
Cannon works with mice given human immune systems, since normal mice cannot get HIV. In one study, she took human stem cells, treated them to have the CCR5 mutation, and injected them into a group of mice, with another set of animals given untreated stem cells as a control. Then she infected both groups with HIV. The result, as published in Nature Biotechnology in July 2010: The control group got sick and died. The mice given the mutation fought off the virus and remained healthy.
Great leaps are still required to find ways to inject the zinc finger nucleases directly into a patient’s body. But an important leap has already been made. Gene therapy is allowing us to imagine a world of Timothy Browns, without everything he had to endure.
News of the Berlin Patient’s cure—Brown stepped forward to identify himself by name only late last year—made its debut at the February 2008 annual Conference on Retroviruses and Opportunistic Infections in Boston. Hütter had submitted a paper to The New England Journal of Medicine and to the conference organizers as well, asking to present Brown’s results—no HIV a year after stopping treatment. The journal rejected his submission, and CROI only allotted Hütter space to put up a poster, the platform offered to present research considered of lesser importance.
Steven Deeks, a professor of medicine at the University of California, San Francisco, and a doctor at San Francisco General Hospital’s Positive Health Program—the newest name for the old Ward 86, the first-ever outpatient AIDS clinic—was among the few to appreciate the significance of Hütter’s display. “I said, ‘Wow, this is interesting. Why doesn’t anyone seem to care?’ ” Another was Jeffrey Laurence, director of the Laboratory for AIDS Virus Research at Weill Cornell Medical College and a senior scientific consultant for AMFAR. “I thought it was the most exciting thing I’d heard about since the discovery of the virus,” he says. “I couldn’t believe people didn’t take notice.” Laurence wrote an editorial about the Berlin Patient in The AIDS Reader. He received two letters. “It basically got ignored.”
Laurence asked Hütter to present his findings to a small meeting of top AIDS researchers at M.I.T. in September 2008. He also asked him to provide Brown’s samples to send to laboratories in the United States and Canada, which could run more sensitive tests. Again, all the samples were negative. Mark Schoofs, a Wall Street Journal reporter who’d been invited to attend the session, wrote an article about the Berlin Patient. The New England Journal of Medicine reconsidered its rejection of Hütter’s paper, publishing his results in February 2009.
The case caught the attention of a small activist organization called the AIDS Policy Project, which was trying to rehabilitate the idea of a cure. One of the things the group does is track the money going to cure research, as a way to highlight the need for more of it. Its founder and leader, Kate Krauss, is an organizer and publicist but not a fund-raiser—the group’s annual budget is roughly the price of a used car. She often travels to scientific conferences by bus.
The Project, together with officials from San Francisco, presented an award to Hütter in June 2010. Stephen LeBlanc, a patent attorney in Oakland active with the group, drove Hütter to the ceremony. He was startled when Hütter told him that this was the first such honor he had received. LeBlanc replied that he’d read that the Berliner Morgenpost newspaper had named Hütter a “Berliner of the Year.” Hütter smiled. “I came in ninth,” he said.
The AIDS Establishment, like many Establishments, tends to be suspicious of outsiders. Here comes a young doctor, not even prominent at his own hospital, who by his own admission knew next to nothing about AIDS, doing something never done before. As more of the research community became aware of Hütter’s claims, the prevailing view was: Who is this guy?
Robert Gallo, a co-discoverer of HIV, devoted his opening address at a major conference in December 2009 to an attack on Hütter’s results. Gallo simply didn’t believe them and warned that only a pathologist could declare the patient cured—once the patient was dead. Hütter, scheduled to speak at the same event, quickly amended his presentation. As he defended his results to a panel of skeptics, he showed the new slide: “Do we have to cut this patient into slices?” it asked.
When Kevin Robert Frost, the CEO of AMFAR, began to cite Hütter’s work in fund-raising pitches, he found that potential donors sought different proof. “They said if the Berlin Patient were true,” he says, “it would be on the front page of the New York Times.”
In fact, the Berlin Patient did appear in the Times—on page A12. The short article included quotes from Anthony Fauci, the director of the NIH’s National Institute of Allergy and Infectious Diseases and the world’s most important gatekeeper of AIDS research. Unlike other experts, Fauci accepted that Brown had been cured. He just didn’t think it was anything to get excited about. “It’s very nice, and it’s not even surprising,” he said—meaning that if you take away someone’s immune system and give him a new one resistant to HIV, it’s logical that he would be cured of AIDS. “But it’s just off the table of practicality.”
It was a disingenuous dismissal: New treatments often start out dangerous, inconvenient, and expensive. It is only with additional research that they gradually morph into, say, a one-pill-a-day therapy that can be administered anywhere, as anti-retrovirals now are. “Picture Alexander Fleming with his vats of penicillin,” says Cannon, “and people saying, ‘Oh, yeah, that’s totally going to work in sub-Saharan Africa.’ ”
Among the big questions remaining about gene therapy is whether all relevant receptors need to be disabled to achieve full HIV resistance. CCR5 is by far the most important of those receptors, but it isn’t the only one, and we don’t yet know how significant this is. With Brown, it didn’t seem to matter. This could be because he had ablation—his immune system was wiped out by chemotherapy and radiation before his transplants. But that raises another puzzle: Could ablation itself be a necessary ingredient to a cure? Full ablation is a punishing experience, and even partial ablation requires hospitalization. No cure is practical on a wide scale if it must employ it.
Science, of course, has ways to find out. Building on Cannon’s work, a clinical trial in San Francisco and Philadelphia is testing whether using the genetic scissors not on stem cells but on T-cells—immune-system cells—to modify them with the CCR5 mutation can also yield HIV resistance. The use of T-cells has some disadvantages, but its big plus is that the procedure wouldn’t require ablation. “If that virus moves, it’s kind of a new universe,” says Jay Lalezari of Quest Clinical Research, one of the trial’s leaders.
Gene therapy is only one possible path to an AIDS cure, and the fact is, it may not be the best one. There is also a less flashy approach, one explored before cure acquired its air quotes: eradication, in which a patient on anti-retrovirals is given an additional drug that wakes up the latent virus so that it can be eliminated. Scientists have identified several different substances that can turn the virus on or off, but so far, none has worked safely in people.
Answers may be years away, but until recently, nobody was even asking the questions. They’re asking now—the International AIDS Society has just set up a working group on an AIDS cure. Despite the early doubters, “the Berlin Patient proved to be a tectonic shift in the way the scientific community looked at this issue,” says AMFAR’s Frost. “I’ve lived it—we started to talk about it internally, then in public. I got e-mails from prominent scientists warning me I was raising false hope. It wasn’t until there was a scientific consensus that the Berlin Patient was cured that people came around.”
If a cure for AIDS is no longer “the C-word,” it’s not yet clear that sufficient money will follow the renewed sense of hope. Gene-therapy research has been almost entirely financed by two new entities: One is Sangamo; the other is the California Institute for Regenerative Medicine, or CIRM, which since 2007 has given out more than $40 million in grants for AIDS-cure research, including $14.5 million to Cannon.
While the pharmaceutical industry has sunk hundreds of millions of dollars into developing AIDS treatments, most drug companies are sitting out cure research. (One big exception is Merck, which is funding studies of some of its drugs’ possible uses in eradication; Gilead is also looking at its compounds for cure candidates.) It’s no mystery why. “The whole field suffers from the lack of a business model,” says Jeff Sheehy, a San Francisco activist and CIRM board member. “A cure may make sense from a public-policy point of view, but not to a company.” Unlike treatment, which must be taken daily for life, a cure would be a one-time intervention. “It’s not that it’s sinister and they don’t want a cure. But it doesn’t fit.”
Drugmakers’ indifference can doom promising potential cures, as compounds owned by a company can’t be used by anyone else. Many AIDS researchers are particularly excited about the eradication possibilities of a substance developed by Medarex. But Medarex was bought in 2009 by Bristol-Myers Squibb, which is testing the compound on cancer but doing nothing visible with it on HIV. (A spokeswoman says the company is “considering the use” of the drug in HIV research, but no trials are set.)
Nor has the NIH’s National Institute of Allergy and Infectious Diseases, the world’s largest funder of AIDS research, made a priority of cure research. According to its own figures—as obtained and published by Krauss—the NIAID spent $40 million on cure research in 2009. That’s 3 percent of its total AIDS-research budget. (Fauci argues that this doesn’t take into account other research that may eventually apply to a cure.) Until recently, the NIAID did not even have an internal code for AIDS-cure work.
But the agency’s reservations about cure research may be softening slightly. Fauci says he hopes to spend some $60 million in the coming year. As of 2013, research networks that niaid funds will be required to include studies directed at a cure. Given Washington’s budget crisis, any increase in funding is noteworthy, and some are choosing to see it as a sign of new commitment. “Tony Fauci is definitely a believer,” says Deeks. He is? “The world has changed,” Deeks says, smiling. “In the past, no. In the future, yes.”
Fauci didn’t seem like a believer when I spoke with him. Gene therapy, he says, is “promising, but it ain’t gonna be easy.” Awakening the latent reservoir? “Nothing that’s a hot product.”
What the NIH spends on cure research “is not even close to enough,” says Frost. “It doesn’t come close to representing the genuine enthusiasm the scientific community feels about the issue—and we risk losing that enthusiasm. The science isn’t all that difficult. We’re closer than people think, and with the right financial investment, we can get there. The real question in my mind is, are we going to find the money to do it?”
Brown’s second transplant cured his leukemia, but it was much harder on him than the first. Neurological problems can be a side effect of the chemotherapy and irradiation used in ablation. In Brown’s case, his doctors suspected that the leukemia had infected his brain and ordered a biopsy. It was negative but brought new trouble. “The surgeons left air bubbles on my brain and had to perform emergency surgery to relieve the pressure,” Brown says. He temporarily lost the ability to walk and talk. Hütter says that CT scans show a scar inside Brown’s head. He cannot pinpoint exactly what happened.
Brown was in physical therapy for more than a year. His intellect is intact, but today he sometimes gropes for words. He still walks haltingly. “My public personality has changed,” he says. “I am not as outgoing as I once was—for better or worse. Part of it is that I no longer feel very attractive.”
In January, Brown moved to San Francisco. His new doctor is Deeks, who is both treating and studying him. Brown is happy to be studied. Aside from a brief stint with ACT UP when he lived in Seattle in 1989, he was never an activist. Being poked and prodded by doctors—and reporters—is his activism now. “I can help,” he says.
Brown’s neurological injuries are of no relevance to the question of how to cure AIDS, but they do serve as reminders of two things we already knew: Ablation is hell, and disease capricious. I asked Brown about living with the knowledge that something has happened to him that has happened to no one else. “I do wonder why,” he says, “but sort of in the same way that I wonder how I got leukemia in the first place. I guess I do not need to ask that question about why I got HIV.” He was twice diagnosed with a fatal disease and cured of both, only to be left impaired—possibly for life, probably by the very thing that cured him. It is not clear whether Brown is the luckiest man in the world or the unluckiest. He’s been lucky for the rest of us.
 |
Illustrations by Matthew Woodson |
Tags:
No comments:
Post a Comment