This is Part II of two parts in my look at PTSD. Part I, which focused on PTSD in the military,
can be found here. This time, we will look at the future of this diagnosis with regard to the DSM-V, the science of PTSD, and a newer approach to treatment.
PTSD in the DSM-V: The Future of a Diagnosis
The creation of the new handbook for psychiatrists, psychologists, and therapists has been subject to
secrecy and scandal. Participants are overwhelmingly psychiatrists (MDs), which contributes to the ever-dominant trend toward a medical model of mental illness (which is true but partial). Many of the docs, estimated at between 2/3 and 3/4 have very strong ties to the pharmaceutical industry, again pushing the DSM toward a more medical model of only including diagnoses for which there is a pill. And to top it off, all participants have signed non-disclosure agreements, essentially swearing themselves to secrecy about the process.
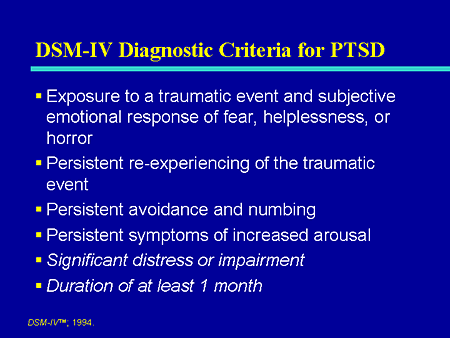
Michael D. Anesti, at the
Psychotherapy Brown Bag blog (a great psychology blog) offers one of the best overviews of the current discussion around how to revise this diagnosis and he provides the current diagnostic criteria from the DSM-IV-TR, which will be useful for the rest of the discussion:
Criterion A: The person has been exposed to a to a traumatic event in which both of the following were present -- the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others
- the person's response involved intense fear, helplessness, or horror (in children, can be expressed through disorganized or agitated behavior)
Criterion B: The traumatic event is persistently reexperienced in one (or more) of the following ways:- recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions (in children, repetitive play may occur in which themes or aspects of the trauma are exposed)
- recurrent distressing dreams of the event (in children, there may be frightening dreams without recognizable content)
- acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur on awakening or when intoxicated)
- intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
- physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
Criterion C: Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three (or more) of the following:- efforts to avoid thoughts, feelings, or conversations associated with the trauma
- efforts to avoid activities, places, or people that arouse recollections of the trauma
- inability to recall an important aspect of the trauma
- markedly diminished interest or participation in significant activities
- feeling of detachment or estrangement from others
- restricted range of affect (e.g., unable to have loving feelings)
- sense of a foreshortened future (e.g., does not expect to have a career, marriage, children, or a normal life span)
Criterion D: Persistent symptoms of increased arousal (not present before the trauma), as indicated by two (or more) of the following:- difficulty falling or staying asleep
- irritability or outbursts of anger
- difficulty concentrating
- hypervigilance
- exaggerated startle response
Criterion E: Duration of the disturbance (symptoms in Criteria B, C, and D) is more than 1 month
Criterion F: The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
Criteria A seems to be one of the biggest battle grounds, as you will see below. Some people think it is too limited and should include other experiences which are not defined as traumatic there
. They argue that divorce or the death of a loved one can produce PTSD, but does not rise to the level of "intense fear, helplessness, or horror." The other side thinks this is just pathologizing a normal response to a "tough" experience.
The broader issue is that at one end are those who want to do away with the diagnosis entirely (some of these people were being encouraged by the Bush Administration and have since become less vociferous) and those who want to expand the criteria to make the diagnosis more widely inclusive. Obviously the extremes are to be avoided.
Here are the real issues, as outlined by Anesti
at his blog:
The criticisms of PTSD stem not from its diagnostic wordiness, but rather contentions that several people have about particular criteria, as well as the underlying nature of the disorder itself. With respect to that latter point, some individuals claim that the PTSD diagnosis pathologizes normal distress. In other words, it is perfectly natural for people to become upset after something traumatic happens, but such distress will run its course naturally. Research has shown, however, that individuals diagnosed with PTSD often still meet criteria many years later (e.g., Morgan, Scourfield, Williams, Jasper, & Lewis, 2003). Such findings indicate that, while being upset by trauma is normal, extreme responses exist that require clinical attention. Other critiques of PTSD center on the symptom overlap it shares with other diagnoses. This, of course is not a problem unique to PTSD. Many anxiety disorders share criteria with one another (e.g., avoidance behavior) and generalized anxiety disorder and depression exhibit a substantial amount of symptom overlap. Nonetheless, the point remains that, to some degree, the PTSD diagnosis might include symptoms that are reflective of overall distress or another diagnosis rather than simply applying to this one specific disorder.
A third critique - the one that has been subject to the most attention - is the inadequacy and utility of Criterion A. In other words, a substantial number of people question whether the diagnosis of PTSD should actually require exposure to a specific traumatic event and a response to that event that was characterized by extreme fear, horror, or hopelessness. Some people argue that this criterion prevents people who meet all other criteria from receiving a legitimate diagnosis and subsequent treatment. Others argue that the broadening of the definition that occurred with the publication of DSM-IV has led to a "criterion creep," allowing for diagnoses of individuals who were exposed to traumatic events that are not viewed as legitimate causes of PTSD (e.g., watching frightening Halloween television programs, losing cattle to foot and mouth disease; Rosen & Lilienfeld, 2008). Research conducted by Breslau and Kessler (2001) revealed that the broadening of Criterion A did, in fact, result in an increased number of PTSD cases, but that the vast majority of those new cases involved individuals learning about the sudden unexpected death of a loved one.
All this being said, there is a fairly strong movement afoot to remove Criterion A in DSM-V. When I first heard this, I was highly skeptical and, in fact, in discussions I have had on this topic with my students in Abnormal Psychology, we have often come to a consensus opinion that this move would not make sense. After reading two articles (one on each side of the argument) in this special issue of the Journal of Traumatic Stress, however, I actually have now changed my opinion. My goal with the rest of this article is to explain the proposed models of these two articles and their justification so that you can make an informed decision as well and lend your voice to the discussion.
Brewin, Lanius, Novac, Schnyder, & Galea (2009)
Brewin and colleagues (2009) propose that the DSM-V should eliminate Criterion A and, in doing so, refocus the diagnosis of PTSD around a specific set of core symptoms unique to this particular disorder. They argue that no other mental illness requires a specific etiology and that, in fact, demanding that a disorder be prompted by a single environmental event while excluding the roles of characteristics of the individual and the interaction of personal characteristics with environment is an overly simplistic way of thinking about mental illness. Indeed, this does seem to discount the idea of the diathesis-stress model. Not everybody responds to the same event in the same way or views particular events as equally traumatic, so requiring a specific triggering traumatic event introduces substantial bias to the diagnostic criteria and shifts focus away from the degree of suffering being experienced by the client. They also argue that, after three revisions of this criteria, we still find ourselves unable to articulate a description that ensures that all appropriate cases are included and all inappropriate cases are excluded. There is little reason to believe this would change in DSM-V.
In the field trials for DSM-IV (Kilpatrick et al., 1998), adjusting the definition of Criterion A to include low magnitude events had almost no impact of prevalence rates. In other words, by creating a situation in which a specific trigger does not have to be identified and events not typically considered traumatic were included, the researchers running the field trial actually did not cause a steep increase in PTSD diagnoses.
Brewin and colleagues (2009) thus believe that, in the DSM-V, PTSD should be based around the core phenomenon of "re-experiencing in the present, in the form of intrusive multi-sensory images accompanied by marked fear or horror, an event now perceived as having severely threatened a person's physical or psychological well-being." In other words, if the individual is having flashbacks of past events, the core of the disorder is present whether or not the individual can identify a specific event that prompted all of his or her symptoms and a response to that event that involved specific emotions. Doing this places an emphasis on the symptoms that are present and are unique to PTSD rather than the individual's recollection of past events and feelings. In this sense, we would become more concerned with treating what is present than in discussing what occurred in the past. To me, this sounds eerily familiar to one of the main arguments for why empirically supported treatments such as cognitive behavioral therapy outperform old fashioned therapeutic approaches like psychoanalysis for so many diagnoses. If people are suffering, it does not matter why as much as it matters how they are suffering and what can be done to improve that individual's quality of life. If PTSD symptoms are induced by something that most people would not view as traumatic...who cares? Perhaps individual differences in variables such as distress tolerance cause particular individuals to experience particular events as more problematic than others. If such individuals exhibit the same core symptoms and will respond to treatment just as well, why not include them in the diagnosis?
Kilpatrick, Resnick, & Acierno (2009)
A second article in the same issue of the Journal of Traumatic Stress arrived at an entirely different conclusion. Like Brewin and colleagues (2009), Kilpatrick and colleagues (2009) acknowledged the imperfections of the PTSD diagnosis and contested the notion of "criterion creep;" however, they believe that the core nature of PTSD requires Criterion A and that revisions are a better answer than elimination.
Their rationale for this suggestion centered on a number of specific points. First, because they believe that PTSD is a disorder that does not occur spontaneously and always follows exposure to some stressful event, removing Criterion A would be inconsistent with the nature of the disorder. Second, they believe that, because the DSM-IV field trails revealed that few people meet the other criteria for PTSD without meeting Criterion A, it makes more sense to simply increase flexibility to include the few cases that might otherwise get lost rather than eliminating the criterion altogether. Third, the authors argued that the better focus is on which events are most likely to induce PTSD, rather than which events should qualify. Ultimately, the authors also argued that revision would allow for a DSM-V criteria set more consistent with prior research on the topic.
Ultimately, these authors acknowledged the imperfections, but believe that revising the criteria while remaining consistent with the research already conducted on this issue makes more sense than a massive reboot of the construct involving elimination of Criterion A.
Anesti changed his mind on Criteria A after reading these articles and agrees that Criteria A should be eliminated, which will greatly expand the possible diagnoses:
the priority should be on maximizing our ability to reliably and validly identify suffering, not on determining a particular event that prompted the symptoms in the first place. Unless research indicates that particular prompting events result in differential responses to particular treatments, what is the point in being hung up on the prompting event? If it is there, and it likely is in the vast majority of cases, it will be clear in the client's flashbacks and nightmares and can thus be adequately addressed in treatment.
I think I agree with his take on it - the most help for the most people.
However, not everyone agrees with that perspective. This article from
The British Journal of Psychiatry looks at some of the issues with the PTSD diagnosis that need to be addressed (in their view) in the DSM-V. They are cynical at best - the reject a specfic etiology (Criteria A) and go on to dismantle the diagnosis on other grounds as well.
Specific aetiology?
Unlike other diagnoses in the DSM that were agnostic to aetiology, PTSD was defined as a disorder that arose after a specific set of traumatic stressors. Thus, the origins of the definition of PTSD rest on the assumption of a specific aetiology (Criterion A). This assumption, already questionable,1 has been undermined by reports that the disorder can develop after a variety of non-life-threatening events (e.g. divorce, financial difficulties).2 Further, recent studies have demonstrated the frequent occurrence of PTSD symptoms among people with depression who had not experienced Criterion A life stressors,3 and among people with social phobias who respond to failed performance situations.4 Even when an individual encounters horrific, life-threatening events (Criterion A), studies find that pre-incident vulnerability factors (e.g. psychiatric history) and post-incident social support contribute more to post-trauma morbidity than does the magnitude of the presumed aetiological trauma.5 In short, Criterion A events are neither necessary nor sufficient to produce PTSD. Instead, they appear to represent high-magnitude stressors that are otherwise indistinct from the full range of stressors that can have an impact on an individual and create risk of psychiatric morbidity. Now set apart from the general field of stress studies, PTSD might arguably be better returned to the fold.
In the absence of a specific aetiology, the rationale for diagnosing PTSD lies in the distinctiveness of the clinical syndrome. This is problematic when one considers that a combination of symptoms of major depression and specific phobia fully constitutes the requisite criteria for diagnosing PTSD.6 This raises the concern that PTSD, at least on some occasions, is simply an amalgam of other disorders. Consider, for example, the case of a boat captain whose fishing vessel is lost at sea, resulting in the death of several crew. Though not physically injured, the captain starts feeling ‘on edge,’ suffers from insomnia and begins to withdraw from usual activities. Most alien to the fisherman’s self-concept, he becomes anxious when considering a return to his usual occupation. Consequently, he turns down offers to work on other vessels, and he becomes isolated from the fishing industry. Without income, this man becomes increasingly anxious and depressed. Prior to the introduction of PTSD in 1980, a psychiatrist would have conceptualised this fisherman’s problems, first, as normal bereavement over lost friends who died in the incident, and second, as a phobic disorder caused by the traumatic event. A third concern would have addressed the development of situational depression as a consequence of adjustment issues and the fisherman’s inability to return to sea. Now, in our post-DSM–III era, we can ask whether the introduction of PTSD has furthered our understanding of this patient’s reactions to a life-threatening event.
It might be expected that ‘traumatologists’ would be cautious in diagnosing a person as having PTSD upon realising that it lacks a specific aetiology and is possibly not a distinct syndrome. Despite that, enthusiasm for the PTSD diagnosis has not been tempered, and the PTSD ‘model’ has been extended worldwide to encompass an increasing array of events and human reactions across diverse cultures. Individuals no longer have to directly experience or witness a traumatic event to be thought to develop PTSD. Instead, based on the DSM–IV, the diagnosis can be provided to individuals who hear of misfortunes befalling others. Peer-reviewed articles have even discussed the possibility of developing PTSD from watching traumatic events on television.7 It has been suggested that rude comments heard in the workplace can lead to PTSD because a victim might worry about future boundary transgressions: the conceptual equivalent of pre-traumatic stress disorder.8 New diagnostic categories modeled on PTSD have been proposed, including prolonged duress stress disorder, post-traumatic grief disorder, post-traumatic relationship syndrome, post-traumatic dental care anxiety, and post-traumatic abortion syndrome. Most recently, a new disorder appeared in the professional literature to diagnose individuals impaired by insulting or humiliating events – post-traumatic embitterment disorder. Even expected and understandable reactions after extreme events, such as anxiety and anger, are now referred to as ‘symptoms’. This expansion of the PTSD model, a phenomenon referred to as ‘criterion creep’, highlights a critical shortcoming of traumatology: the cross-cultural medicalisation of normal human emotions.9 Labelling situation-based emotions and upsetting thoughts as ‘symptoms’ is akin to saying that someone’s cough in a smoky tavern is a symptom of respiratory disease. Such illogical leaps increasingly inform our cultural narratives when we discuss human reactions to stressful events, possibly giving rise to iatrogenic misapprehensions and contributing to chronicity. Not only has the PTSD model been expanded, but patients who present with psychiatric problems after traumatic events increasingly receive the diagnosis. Perhaps in this time of managed care, physicians have come to believe that without a PTSD diagnosis a patient’s reactions to traumatic stress will be denied appropriate psychiatric attention, therapeutic intervention, and proportional compensation. Pressure for a PTSD diagnosis also may arise when patients are involved in personal injury claims. Unlike depression or other psychiatric diagnoses that can be caused by multiple stressors unrelated to a legal claim, a PTSD diagnosis is incident-specific and clearly determines causation. Unfortunately, what may be best for a lawsuit is not necessarily best for the patient. By narrowing a physician’s analysis of causation to a single event, a PTSD diagnosis may downplay or even ignore crucial pathogenic features that are to be found in the broader context of a patient’s personality, developmental history, and situational context.
Implications
In light of these research and clinical considerations, psychiatrists should consider alternative perspectives and the full context of a patient’s presentation when formulating their diagnosis. The diagnosis of PTSD may be appropriate in some cases, but physicians should not provide it reflexively in the aftermath of trauma. As for the DSM–V, it is unclear how current problems can best be resolved. In observing the issues that have followed PTSD since 1980, we are not dismissing the diagnosis, nor are we ignoring a wealth of research findings spurred by the construct. Rather, we are asserting that there are reasons for concern. Defining PTSD criteria in DSM–V so that they reflect current findings, while limiting the construct’s susceptibility to misuse, expansion and reification, will be a difficult challenge.
It is good that they do not totally reject the diagnosis, especially because as we saw in
Part I of this series, military veterans are exhibiting very intense symptom patterns that not only justify the diagnosis, but are teaching us a lot more about the disorder.
The Science of PTSD
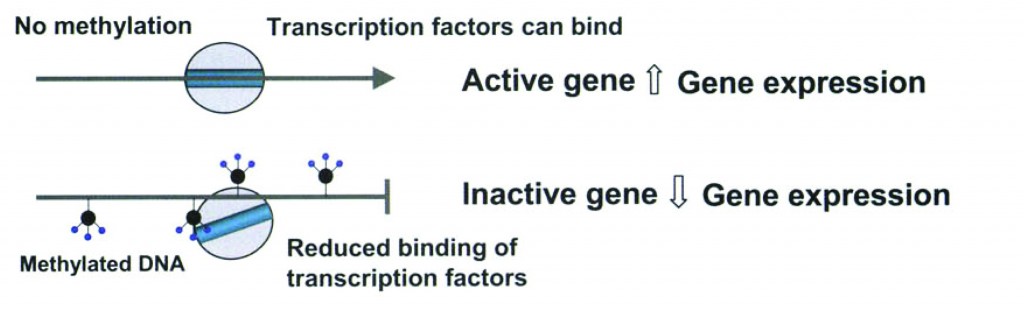
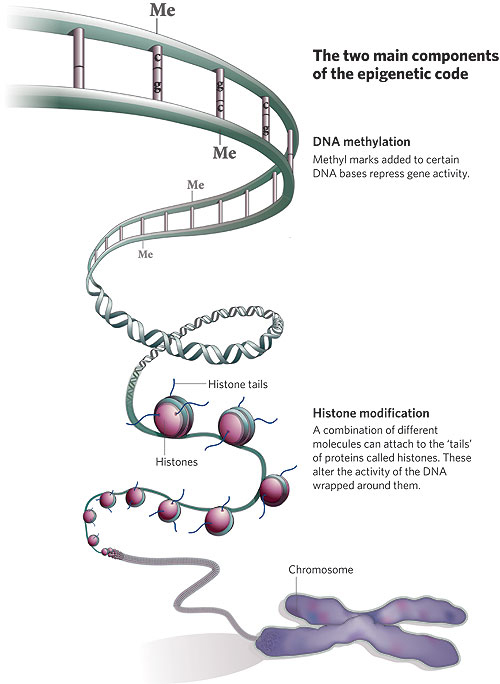
Regardless of the diagnostic criteria, there is a great deal of
neuroscience evidence for PTSD, including an enlarged amygdala and a shrunken hippocampus:
A great deal of research has attempted to identify those parts of the brain whose function may be altered in PTSD. Three key areas have been identified, the prefrontal cortex, amygdala and hippocampus. Much of this research has utilized PTSD sufferers from the Vietnam conflicts. For example, a prospective study using the Vietnam Head Injury Study showed that damage to the prefrontal cortex may actually be protective against later development of PTSD[26]. In a study by Gurvits et al., Combat veterans of the Vietnam war with PTSD showed a 20% reduction in the volume of their hippocampus compared with veterans who suffered no such symptoms.[27]
In human studies, the amygdala has been shown to be strongly involved in the formation of emotional memories, especially fear-related memories. Neuroimaging studies in humans have revealed both morphological and functional aspects of PTSD.
The amygdalocentric model of PTSD proposes that it is associated with hyperarousal of the amygdala and insufficient top-down control by the medial prefrontal cortex and the hippocampus particularly during extinction.[28] This is consistent with an interpretation of PTSD as a syndrome of deficient extinction ability.[28][29] Further animal and clinical research into the amygdala and fear conditioning may suggest additional treatments for the condition.
The amygdala is our first order emotional processing center. It is here that events are paired with emotions - especially fear related memories. In PTSD the amygdala is over-aroused (and enlarged) and the hippocampus, which would normally modulate and contextualize the emotional memories, is less active and has been noted to shrink.
Yet how this happens is a mystery. The Wikipedia entry cited here suggests that low cortisol may be to blame, though that is unclear.
Perhaps no one is better known in the trauma treatment and research community than
Bessel van der Kolk. Here is the abstract to an article he published in 2006 (
Clinical Implications of Neuroscience Research in PTSD. Ann. N.Y. Acad. Sci. xxxx: 1–17):
ABSTRACT: The research showing how exposure to extreme stress affects brain function is making important contributions to understanding the nature of traumatic stress. This includes the notion that traumatized individuals are vulnerable to react to sensory information with subcortically initiated responses that are irrelevant, and often harmful, in the present. Reminders of traumatic experiences activate brain regions that support intense emotions, and decrease activation in the central nervous system (CNS) regions involved in (a) the integration of sensory input with motor output, (b) the modulation of physiological arousal, and (c) the capacity to communicate experience in words. Failures of attention and memory in posttraumatic stress disorder (PTSD) interfere with the capacity to engage in the present: traumatized individuals “lose theirway in the world.” This article discusses the implications of this research by suggesting that effective treatment needs to involve (1) learning to tolerate feelings and sensations by increasing the capacity for interoception, (2) learning to modulate arousal, and (3) learning that after confrontation with physical helplessness it is essential to engage in taking effective action.
I mention this article because he makes some important observations about the neuroscience of PTSD that has not been widely acknowledged either in treatment of the disorder or in its defintion.
Neuropsychology and neuroimaging research demonstrate that traumatized individuals have problems with sustained attention and working memory, which causes difficulty performing with focused concentration, and hence, with being fully engaged in the present. This is most likely the result of a dysfunction of frontal–subcortical circuitry, and deficits in corticothalamic integration.[22,23]
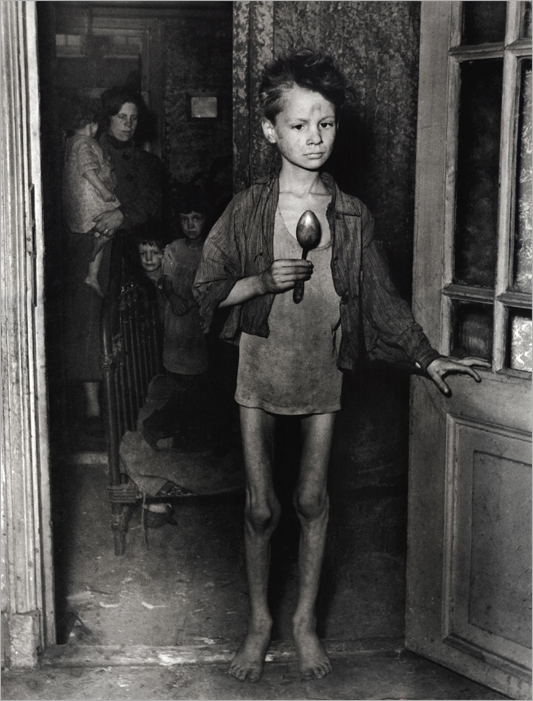
Many traumatized children and adults, confronted with chronically overwhelming emotions, lose their capacity to use emotions as guides for effective action. They often do not recognize what they are feeling and fail to mount an appropriate response. This phenomenon is called “alexithymia,”[24] an inability to identify the meaning of physical sensations and muscle activation. Failure to recognize what is going on causes them to be out of touch with their needs, and, as a consequence, they are unable to take care of them. This inability to correctly identify sensations, emotions, and physical states often extends itself to having difficulty appreciating the emotional states and needs of those around them. Unable to gauge and modulate their own internal states they habitually collapse in the face of threat, or lash out in response to minor irritations. Futility becomes the hallmark of daily life.
Psychology and psychiatry, as disciplines, have paid scant attention to the deficient orientation and action patterns that are triggered by sensory input, and, instead, tend to narrowly focus on either neurochemistry or emotional states. They thereby may have lost sight of the forest for the trees: both neurochemistry and emotions are activated in order to bring about action: either to engage in physical movements to protect, engage, or defend or displaying bodily postures denoting fear, anger, or depression that invite others to change their behavior. Pharmacotherapy helps to address some of the neurochemical problems associated with PTSD, thereby helping to modulate some of the embarrassing and upsetting behaviors and emotions, but drugs seem to not really be able to correct whatever abnormality underlies these behaviors and emotions. (pg. 4-5)
[For those interested, you can read a wonderful collection of his articles at this site (most of them are PDFs).]
According to van der Kolk, neither cognitive behavioral therapy (CBT) protocols nor psychodynamic approaches (the two main treatment approaches for trauma) pay sufficient attention to the experience and interpretation of disturbed physical sensations and preprogrammed physical action patterns. With this in mind, he has studied and advocated from more somatic-based treatments, including Eye Movement Desensitization and Reprocessing (EMDR) in treating PTSD - see
here,
here, and
here, for example.
For more on the biological/neurological aspect of PTSD, see this great article from van der Kolk:
The Body Keeps The Score: Memory & the Evolving Psychobiology of Post Traumatic Stress.
Dissociation in PTSD and its Treatment
One of the overlooked elements of the PTSD diagnosis that needs to be integrated into the definition is the degree of
dissociation involved. Dissociation occurs on a spectrum from very mild (daydreaming) to very severe (
dissociative identity disorder).
Some authors contend - and I agree - that dissociation has not been recognized as a central element in PTSD, or at least in Complex PTSD.
From
Dissociation: An Insufficiently Recognized Major Feature of Complex PTSD by Onno van der Hart, Ellert R.S. Nijenhuis, and Kathy Steele: Journal of Traumatic Stress, 2005, 18(5).
It is difficult to determine whether “dissociation” is a central feature in complex PTSD and other trauma-related disorders because there is not uniform agreement on what constitutes the construct. The current use of the term is highly confusing (cf., Marshall, Spitzer, & Liebowitz, 1999). For example, some PTSD intrusive symptoms are referred to as “dissociative flashback episodes” (APA, 1994, p. 428), while the same flashbacks are not described as dissociative in ASD. The PTSD diagnosis does not consider avoidant or numbing symptoms to be dissociative, but in ASD these very symptoms are labeled dissociative (APA, 1994, p. 432). In the trauma literature at large, there are debates about whether or not dissociation is dimensional or a taxon, and which symptoms should be included under the rubric of dissociation. In relation to dissociation and trauma-related disorders in general, and complex PTSD specifically, we thus briefly introduce a theory regarding the processes and manifestations of dissociation that recommends a way to clarify this conceptual problem.
As part of this theory, we will define the term “personality;” describe the induction of structural dissociation of the personality during traumatizing events; illustrate the characteristics of parts of the personality that are dissociated to some extent from each other, and are fixed in enduring maladaptive behaviors and ways of perceiving, and in avoidance or reexperiencing; describe levels of complexity of this structural dissociation; and discuss the scope of dissociative symptoms stemming from structural dissociation, and distinguish them from what we consider to be related but non-dissociative phenomena. Finally, we analyze a number of symptom clusters of the proposed diagnostic category of complex PTSD/DESNOS in terms of structural dissociation of the personality, proposing that they all potentially involve dissociation. (pg. 2)
Here is how this study looks at the dissociative process in trauma survivors:
Our hypothesis is that integration between defensive and daily life action systems will fail first and most readily in a context of extreme stress that reduces integrative capacity. This integrative failure basically manifests in the prototypical alternations between functioning in daily life with avoidance/numbing (daily life action systems), and reexperiencing (defense action systems). We also hypothesize that survivors may develop a phobia of reexperiencing if they do not integrate these intrusive and intense trauma-related memories. This phobia sustains ongoing dissociation of daily life and defensive action systems. (pg. 3-4)
The way they conceptualize this happening is very similar to ego states work (Watkins & Watkins, 1997) or Internal Family Systems "part work" (Schwartz, 1995) and various other methods of working with what are variously known as complexes (Jung), ego states (the Watkins), parts (Schwartz), or subpersonalities (Rowan). [
Emphasis added below.]
The basic pattern of posttraumatic stress response can be described as an alternation between a single dissociative part of the personality mediated by action systems of daily life and a second (rather limited and rudimentary) part mediated by defense. When the major dissociative part of traumatized individuals is detached from the trauma and mediated by action systems of daily life, the individual can seem rather undisturbed and able to lead a (relatively) normal life. However, this normality is only apparent, because this part of the personality physically and mentally avoids trauma-related cues, including his or her intrapsychic world, resulting in life “lived on the surface of consciousness” (Appelfeld, 1994, p. 18). Parts fixated in action systems of defense tend to intrude or become dominant when the individual is confronted with major threat cues. (pg. 5)
The first and best thing about this approach is that is does not pathologize the clients - they are wounded human beings with a dysfunctional part - the traumatized part. Yet it also provides a more somatic approach to treatment, for which van der Kolk is advocating, in that the various forms of parts work or ego states work can also work with the body.
And yet, seeing how the new DSM is being constructed, the medical model would never admit such an approach. Even in the managed care system, only treatments like CBT, which
van der Kolk has shown to be inferior to somatic based approaches like EMDR, or
brief therapy are covered by insurance most times.
The Future of PTSD
There is no doubt this diagnosis will survive the next few rounds of revision in the DSM. However, with the DSM becoming more and more dominated by the medical model and with treatment also quickly moving in that direction, the more effective treatments for PTSD will remain on the fringe of the therapeutic community.
On the bright side, the military is experimenting with EMDR and with Schwartz's parts work in treating soldiers. The dark side of this is that they are seeking faster ways to return their weapons of war to active duty and hoping these alternative approaches might do the job.
If they turn out to be more effective than drugs or CBT, they will likely make their way into the mainstream - or at least that is what we can hope.
Tags:
Psychology, PTSD, anxiety, trauma, therapy, The Shadow of the Millenial Decade, Bessel van der Kolk, EMDR, dissociation, DSM-V, Michael D. Anesti, Psychotherapy Brown Bag, DSM-IV-TR, Criteria A, The British Journal of Psychiatry, etiology, neuroscience, amygdala, hippocampus, CBT, The Body Keeps The Score, Memory, Psychobiology, Complex PTSD, parts, Richard Schwartz, ego states, somatic approach to treatment